Clostridia perfringens
otherwise known as
GAS !

Where do we begin? Rinnnnnnnnng . . . . .
Maybe with a telephone ringing. Hospital rounds went well.
You have just gotten to your office.
Patients are being processed and placed in exam rooms.
But that's the emergency line and you are not on call. Odd.
It's the hospital's admitting pediatric resident
with an important question.
She apologizes, she knows you are not on call,
and the patient isn't yours, but something came up that sounds
a bit like something you lectured on two months ago. She's very tempted to push the panic button.
You interject, Just curious, whose patient is this?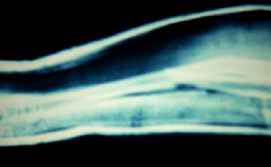
Dr. Mia. They have looked and called everywhere and can't find him. He made
rounds before 6:00 this morning and said something about his 'flight' - whatever that meant. His 14 year old patient fell off a swing yesterday onto grass and
broke his left forearm - both bones - with a small 'in out' puncture wound near the ulnar bone part of the fracture. That's what is described in the brief op note.
He was taken to surgery yesterday evening - not long after being seen in the emergency room. We have notes.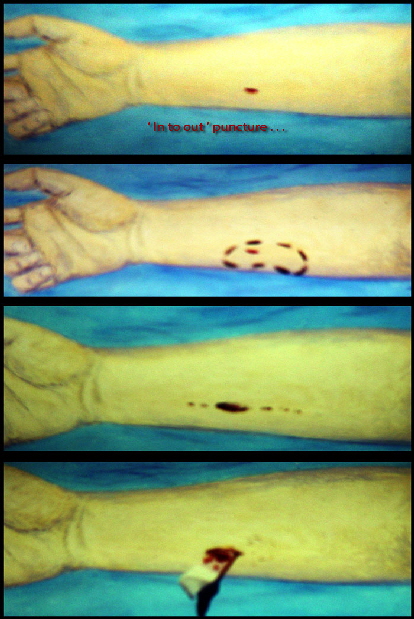
There was 'some undermining' just inside the puncture - those are the words he used... so he elliptically excised the puncture to make the wound able to accept a rubber
ribbon drain (about 1.5 cm) and he also split the fascia deep to the skin to decompress the area.
<=(These are later drawings based on the descriptions)
Undermining under skin (dotted oval).
Dotted line is path of subcutaneous split made in the fascia extending 3 cm proximal and 2 cm distal.
Through this was ' copious irrigation ' squirted in and sucked out.
A rubber drain (thin collapsible tube) vents deep drainage to the surface.
IV antibiotics (Cephalosporin) were given and ordered for 24 hours at 8 hour intervals.
A reduction was carried out and cast applied to hold the reduction.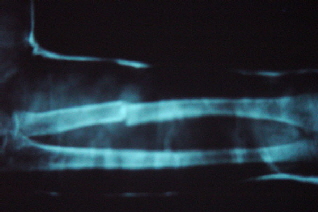
 The reduction was described as
The reduction was described as
'near perfect' as seen in several views by x-ray. He was admitted to pediatrics post surgery for his antibiotics and for some pain management.
From Dr. Mia's note written just before 6:00 am there was some expected throbbing and good capillary refill to the fingers. No fever was noted although the morning temps had not yet been gathered.
This typed dictated note was not back from transcription for several days.
 |
The description is close to what was written - a total fasciotomy
(cutting the cloth-like tube that surrounds the muscle compartment) of 5 cm,
2 of which was distal and 3 aimed proximal.
What's the question?
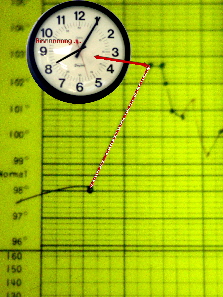
He has suddenly become much more anxious, weird acting and seems hard to keep comfortable.
What happens when you extend his fingers?
Don't know.
Do it. I'll wait on the line.
OK. Oh by the way his temp has spiked to 102.6 F. . . . puts phone down... pause . . .
Over the phone, from seemingly very far away, is heard a horrendous scream echoing in the corridors.
The office nurse is told to hold this phone line open, tell the resident when she reports back, to get that patient to the operating room immediately and have his mother meet me there. Call on the other line to set an operating room open for immediate
surgery and notify the following people (list given). .. When the resident returned to the phone she related the scream we
already figured was his. She complies with the request to get the patient to the operating room immediately. Eight minutes later
mother is stuttering and blindly signing consents as we are already into the room with cast cutters getting the cast off. Mother was told - if we discuss this your son dies. Period.
I don't know if I can save the arm.
As the anesthesiologist crashed the patient the drain was pulled to release a strong
belch of nasty fluid. Here put a swab of that into a blood drawing test tube filled 2/3s with milk from the O.R. coffee pot area. Plug it with Vaseline gauze and sit the
test tube in a some coffee to make it warm. Don't put anybody's face near the test tube as it will probably blow.
Less than 15 minutes later the greased gauze shot out. Diagnosis of Clostridia
perfringens made with certainty. The forearm was already filleted and power tools used to remove the broken ends of the forearm bones which had many fine green lines running in tiny canals for about one cm
from the broken ends. Holes were drilled into the bones to allow reverse flush of the marrow. Every muscle was exposed and
washed and gallons of mixed saline and peroxide were everywhere. Maintenance helped housekeeping squeegee the floor into
high volume suction which was set up as the floor became a lake. Every person in that room stripped to the minimum and was hosed off and re-gowned at least 4 times before the process had run its course.
Bacteriology called to confirm that gram positive rods with spores were seen. Pathology confirmed that some of the green
tissue sent was "definitely plant, can't say grass exactly but probably". The skin edges opened from palm of hand to elbow
were gaping about 8 inches apart with a football sized swollen mass of muscle bulging out. Antibiotics included Gentamycin
and three kinds of penicillins (as much as we could get as fast as we could give it -as quoted the anesthesiologist).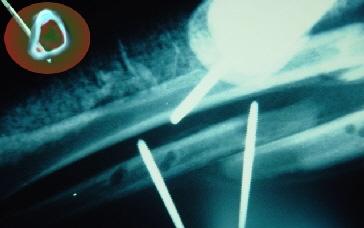 K-Wires (threaded pins) were drilled into bone away from the fracture area from the skin side of the forearm and placed so as
not to block the marrow cavities - 'cortical placement'. The bones were placed bayonet style (back to back side by side) so not to occlude marrow drainage. Ready external fixators
were not (back then) available so the pins were placed through plastic shipping tubes which were then filled with methacrylate plastic - a fast hardening plastic found in operating rooms.
K-Wires (threaded pins) were drilled into bone away from the fracture area from the skin side of the forearm and placed so as
not to block the marrow cavities - 'cortical placement'. The bones were placed bayonet style (back to back side by side) so not to occlude marrow drainage. Ready external fixators
were not (back then) available so the pins were placed through plastic shipping tubes which were then filled with methacrylate plastic - a fast hardening plastic found in operating rooms.
Early next morning and every morning thereafter he was given anesthesia and the dressings all changed and tissues inspected. The upper arm was explored for lymphatics and found to be
OK. That wound was closed. Even a small rise in temperature from normal meant a trip back to the operating room. There
were 19 trips in all. As 'granulation' filled in the spaces between the muscles that was being kept open by loose gau ze fluffs the gauze was advanced out slowly. We waited for the crevices to fill in so that skin graft could be placed without any deep pockets
beneath. The area near the original puncture wound was last to fill in. It was also noteworthy that the ulnar nerve was found to be apart and was woefully infected at the edges and needed to be
trimmed to clear infection. Fortunately this youngster had a rare finding called 'median dominant hand' wherein nearly all the hand innervation that would normally come by way of the ulnar nerve
was instead coming by way of the median nerve.
ze fluffs the gauze was advanced out slowly. We waited for the crevices to fill in so that skin graft could be placed without any deep pockets
beneath. The area near the original puncture wound was last to fill in. It was also noteworthy that the ulnar nerve was found to be apart and was woefully infected at the edges and needed to be
trimmed to clear infection. Fortunately this youngster had a rare finding called 'median dominant hand' wherein nearly all the hand innervation that would normally come by way of the ulnar nerve
was instead coming by way of the median nerve.
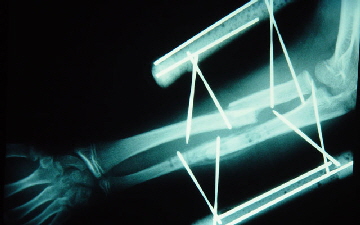
Bone healing side by side is actually quite fast and reliable. See for yourself.
You can see that there is bone healing already bridging the bone
fracture area well before the muscle swelling has gone down and grafting completed.
Left over k-wire pieces inside the plastic tube filler, seen on x-ray,
help stiffen the construct. Nonparallel pins also make for more stability at a safe distance.
Skin grafting uses mesh which allows a smaller area of donor skin than the area to be covered. It also allows drainage
through the many spaces in the mesh so that the graft does not get floated on liquid that can become infected.
Here is the most important anatomy lesson in all of medicine.
Bacteria do not have teeth.

Got that? No teeth. They can't chew. They don't swallow food whole or in chunks. To digest their food they need to secrete their digestive enzymes into their environment. Any pocket that holds fluid in a pool becomes a bacterial stomach and feeding ground. THIS IS WHY SOAP WORKS!!! You wash away the little bas$ %S ability to eat! Wash secretions (potential nutrition and digestive enzymes) away and denature them with a great denaturing substance - soap. So washing is key. Constantly getting rid of enzyme saturated ooze starves bacteria.
He is smiling. He knows that he is killing the nasty beasts that tried to kill him.
That's a big soapy tub that churns and washes the ooze away. The dressing on the left thigh covers the skin donor area which is actually half the size of the dressing.
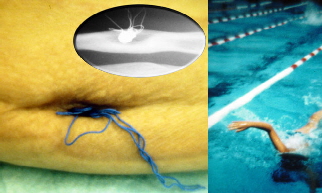 Operation 19 was to open wider one small pocket that did persist, drill
it through & through to allow granulation from the bottom to heal up from the depths and that was that. Notice how well the bones are reshaping despite bayonet position originally. Good enough for
swimming which is what he was best at before all of this.
Operation 19 was to open wider one small pocket that did persist, drill
it through & through to allow granulation from the bottom to heal up from the depths and that was that. Notice how well the bones are reshaping despite bayonet position originally. Good enough for
swimming which is what he was best at before all of this.
 |
A really trained eye can see the very mild 'benediction' open hand that gives away partial ulnar nerve loss. Functionally, he returned to sports including tennis and ocean sports including water skiing.
How did we KNOW, sight unseen, that we had Clostridia perfringens while on that phone? Only two organisms can make that kind of fever in 18 hours, Clostridia and strep. The scream (on having his fingers extended for him) was a definite indication of compartment syndrome - a vascular disaster all of its own. Deep small wound, high abrupt fever = gas until you show it isn't. Thanks to Dr. John Kelly Smith who many years ago taught the trick of incubating milk in a test tube for rapid verification of C perfringens hours before lab methods and the subtle differences in putrid smells - with practice practice practice.
Why no hyperbaric oxygen?!?
Hyperbaric oxygen kills - two ways. Speed to stop Clostridia and REMOVE IT as it chugs out many poisons... is more important. People die because of delay caused by getting hyperbaric services arrange and transfer to facilities that may or may not have somebody there ready to go. In the extremities we can open everything wide enough to get that job done and do so very fast (peroxide in the wash water provides an extra very high oxidation boost as well).
Once the critters make it to the BODY cavity it is another story. We can't fillet the intestines or chest cavity and flush air everywhere. One sailor case required opening his skin all the way to the nipples from the gangrenous leg with which he arrived and which was quickly amputated. The infection did not go deep into his core body cavity and so the surface was enough. For safety, the follow-up next clean out was done in a real hyperbaric oxygen chamber wherein his wounds were tended to by a resident doctor who then seized and died in that chamber. Did we mention that hyperbaric chambers can kill? That's right, the doctor died. There is a percentage mortality with being in real hyperbaric chambers - sick or otherwise. [there are many make believe units out there that are not the real deal and are safer but probably placebo].
Another very effective way to quickly stop gas gangrene is with dry ice. It essentially does immediate physiologic amputation. After the patient gets well, generally quite quickly after the infected part is frozen, the frozen part needs to be surgically amputated . The dry ice reduces the mortality of delay and anesthesia associated with malnutrition and gas gangrene that has not gotten to the body core. It stops the poisons which shut down the nervous system , heart and kidneys. People come out of coma in minutes after the infected part is frozen.
So where is Clostridia pefringens? EVERYWHERE. Just about any place where there is dirt. It is a very common bacteria. So why don't we see more cases of this type? The key is that this bacteria is inhibited by oxygen. It is an organism of decay. It likes in dead tissue and helps get it that way with nasty toxins (alpha toxin is the famous one that zips through muscle). Swallowed clostridia can produce gut damage with beta toxins. Would you believe - seriously - there are people who use clostridia making gas to raise bread! Yuk The cooking kills the buggers but what if - mmmmm - it were under cooked? Yeast works fine and is much friendlier to people, thank you. What is dangerous is the idea of making this diagnosis by culture. THAT TAKES TOO LONG! WAY TOO LONG! That is autopsy stuff. Safe bet is leave dirty wounds open. Not only do not get them stitched, get them opened MORE if deep and potentially dirty. The military axiom is that there are no small penetrating wounds at least not for long - medics will see to even before transport.
Food poisoning is a topic for somebody else's web site.
I would like to thank Dr. Storer & Dr. May of Yale for their teachings reflected here and Dr. Arthur Pappas (at that time of
Harvard) who drilled this stuff into my noggin (with a smile). Dr. John Kelly Smith was the first (was at Cornell Med NY
Hospital ) to teach the practical tricks of early detection of Clostridia including smell training sessions with a variety of fresh
killed organisms), shirt pocket or coffee cup incubators and the like. Thanks to the U.S. Navy for the practical real world access to this condition, - - - could have been nicer without the war, though.