More about fractures...
 |
They teach you in school all about Babylonians. That's cool. And um those Crow Magnum fellows (drank a lot, huh?). Now, if you get those facts muddled, who even notices, and, what bad happens?
What's the point? Well, chances are you will never meet a Babylonian nor an extinct hairy guy who looks like your mother's brother. But - you will be called on to help out or make a decision on some child's broken bone. The schools just do not prepare you for reality. That is what this section is all about, not bone fine details, but savvy.
Bones are not calcium. Sharks have bones with nearly no calcium. Bones are stiff structural thingies with fairly complex structure. As with shirt collars, they may be starched (stiffened with calcium in our case) or not. Children's bones are in large part like shark bones, largely cartilage. Let's look at kinds.
Membranous bone. These are plate-like bones. Bones in sheets. Your skull is made up of these linked in puzzle like edges when your head stops growing. They float in children to allow the brain to grow and grow themselves within their membranes.
Teeth. Teeth are teeth. Look up a dental web site. Not our interest here. But brush and floss regularly.
Short Bones. There are quite a few bones made of cartilage which grow circumferentially. That is, they just get bigger all over. The wrist and mid foot bones are examples. Basically the proportions of shape stay about the same. Growth is a generalized process. For this to happen, these bones must remain predominantly cartilage until late in growth. They start to close down growth from the inside out by developing bone (the calcified substance) in the center. That bone transformation from cartilage spreads outward to take over the entire "bone" (the structure). A single complex bone - a vertebra - will convert from cartilage to boney in composition from several regions within its structure at once. Those centers of expanding transformation join up. So how does this happen? Magic. Well magic and blood vessels. Cartilage does not contain blood vessels. Cartilage is kind of like Jello, in that it is very porous to water. Nutrients ooze in and through. Bone is formed by an invading blood vessel which organizes the boney transformation as the vessel branches out like a tree within the cartilage. The magic is in the chemistry triggered by the blood vessel which causes cells to take on new roles.
When such bones are broken, the key question is what happened to the trunk of the tree which is within the bone. If that arterial trunk is sheared, then healing won't occur until and if that vessel gets repaired. Oblong short bones which have only one main arterial trunk are most likely to delay in healing if fractured as one can bet the fracture shears the main blood inflow route.
Long bones. These are the lanky ones - humerus, radius, ulna, femur, tibia, fibula, finger and toe bones etc. They are in part, kind of membranous as the long shafts get fatter by bone made by the surrounding membrane (periosteum, peri=surrounding, osteum= the bone). But the bones get longer by means of special plates of growth cartilage at the ends . This isn't too unlike tree branches growing longer by buds at the ends and getting fatter by appositional (additive) growth beneath the bark.
This is important. Children are growing. Adults are not. So children have these growth features and structures and adults do not. Children have a membrane, periosteum, around their bones. It runs as an enveloping tube, like the skin of a sausage, from end to end - from end growth plate to other end growth plate - with some variations. When an adult bone breaks, it tends to go all over the place whereas the durable periosteum of children's bones tend to maintain some sort of proximity. Also, the periosteum creates a continuity. The bones may be broken "apart" on x-ray, but the periosteum probably still spans the broken pieces. That tube of periosteum may be torn and stretched, but it usually still spans. That's why kids bones heal so well, in any position or angle. We do not set bones to make them heal in children. They will heal. It is how they will heal.
The tissue that surrounds the bones has the uncanny ability to seek the original shape to a variable degree. We do not need to torture children to get 100% or "anatomic" bone settings. The younger the child, the more it can undo fracture deformity all by itself. And the problem is that if you do manipulate to perfection, how do you hold it?
Ay. There's the rub. Healing isn't the problem. Circulation and nerves and really
important stuff that does not show on x-ray may be badly hurt by efforts to hold perfection of bone pieces when the bones are the most able to fend for themselves. Casts
so tight as to be certain to hold bone perfection are tight enough to allow loss of limb altogether. Learn that! Bones are just bones. Bones are forgiving. We can screw them up
and they come back. We can let them heal badly positioned and get a later chance to make them pretty. We do not get second chances with circulation. Decision making in
treating children's fractures is NOT even a little bit dominated by bone healing. It is all about keeping things alive, not  damaging things further, and knowing when to defer and
when to get hopping.
damaging things further, and knowing when to defer and
when to get hopping.
First of all, bone fractures do not even begin to join up for well over 10 days (less in infants). An immediate rush to bone setting does not shorten healing time by even a second. Bones set five days after the fracture happens will be healed at the same time as if they were set immediately.
What happens first is delivery of healing materials to the fracture site and removal of debris, then when everything is ready, actual knitting takes place.
Reasons to move quickly :
* Something else (a liver, a spleen, head etc.) was also injured which requires moving quickly. Tag along.

* Displacement of tissue is impairing circulation by stretching or kinking an artery or veins
are being stretched such that return flow is daming up..
 * Swelling is creating back pressure which impairs venous blood flow. That,
will, if the return is slowed enough, slow the arterial inflow. There are compartments within the limbs. Flow may be slowed to a stop in one compartment but be normal in another. The single most telling thing that blood
flow is impaired and that a real emergency is at hand is horrendous pain. Now we have to get real here. We can't cry wolf. Every fracture hurts. But usually if the youngster holds still, they are consolable. Not so with
circulation loss.
* Swelling is creating back pressure which impairs venous blood flow. That,
will, if the return is slowed enough, slow the arterial inflow. There are compartments within the limbs. Flow may be slowed to a stop in one compartment but be normal in another. The single most telling thing that blood
flow is impaired and that a real emergency is at hand is horrendous pain. Now we have to get real here. We can't cry wolf. Every fracture hurts. But usually if the youngster holds still, they are consolable. Not so with
circulation loss.
In elbow fractures, the kids - even when crying - can be asked to wiggle their fingers or have them gently uncurled without much discomfort. When that simple act is vile in its painfulness, then circulation loss has to be assumed and an emergency is present. This is evidence that the muscles in the deep compartment (the most at risk place) are lacking blood flow. That same deep compartment houses a main nerve. Fingertip circulation may even be good. Pink finger tips and nail bed color cannot be relied on as the last word.
* Open wound, with exposure of damaged tissue to bacteria. The hurry is not to set the bones but to clean the tissue. Frequently, when fractures are soiled, setting the bones is deferred for many days while wound care is in process. Setting the bone might in certain cases even impair a second look clean-out.
Reasons NOT to move quickly :
* If a child has a belly full of food, then anesthesia (if anesthesia is needed) becomes far
more risky. Circumstances may dictate shorter or longer waits.
* The appropriately skilled persons or needed equipment are not available. As long as circulation is not threatening, one can wait days. In order to not allow the tissues to twist
or stretch and FOR COMFORT, a splint may be used. A splint that increases pain may have gotten too tight from swelling within. Even casts that are fine when first applied, may BECOME tight as swelling occurs.
* Cast too soon and the cast will become too tight, creating an emergency to get it off. Cast over too swollen an area and the cast becomes uselessly loose as the swelling
subsides. Very often splints are used initially because they can accommodate both swelling and shrinkage of swelling.
* Bad skin. If surgery is required due to the specifics of the bone injury, a major fear is infection. That risk goes way way up if the skin is mauled or tattooed with grime. Sometimes we need local anesthesia or a cream anesthetic topically to clean such skin. To operate through bad skin only increases risks with very little promise of better outcome. Often we wait five or six days until skin is healed and swelling on the way down. Here is an option when very poor skin is present (say a car wheel ran over the ankle directly and it isn't clear that skin grafting may be needed. Let the bones heal as they are. And even a month later, surgically recreate (we can do that) the fracture under sterile and optimum conditions and get it all lined up. A surgical fracture shortly after a real fracture will heel in about half the time as the needed metabolic process is already up and running.
Growth Plate Fracture
IS that bad?
Sounds bad, doesn't it? Actually it can be very nasty. However, like being hit by lightening it isn't good but it is rare. Growth plates are constructed with a built in break zone (like paper towels). Most of the kiddy fractures of the growth zone do just fine. The important point is that it isn't the actual fracture that makes the trouble. It is grinding compression of the growth cells - linear impact that does that damage. Traction and twists usually fail at the safe zone. Compression injuries might not even have fractures. Many a growth arrest occurs in the "other" bone - the one that was not broken. We just cannot tell if there is compression damage to that zone at the time of initial treatment. Just have to wait and see.
Fractures that CROSS the growth plate, like land in a earth quake that winds up at two levels is quite bad. If a growth plate winds up like this: =========== then surgery is needed to put it back or else bone will cross the defect and weld the plate. Depending on how big a weld and how much growth remaining, the growth may stop altogether, or curve around the weld or sink in like a sink hole.
Joints
Fractures that enter joints can be real trouble as well. Joint surfaces that are not smooth will grind and self destruct over time with use. Disturbed joint surfaces require repair.
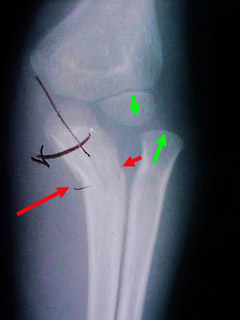 However, fractures that distort joints or even dislocate them also get our attention. At the right, an elbow joint has the upper arm bone (humerus) intact. The forearm
bone called the ulna is cracked (between the red arrows) and bent but not apart. It is broken like a green stick. Actually it is quite solid at the fracture area.
However, fractures that distort joints or even dislocate them also get our attention. At the right, an elbow joint has the upper arm bone (humerus) intact. The forearm
bone called the ulna is cracked (between the red arrows) and bent but not apart. It is broken like a green stick. Actually it is quite solid at the fracture area.
The other unbroken bone (the radius) has been levered out of its joint. It is dislocated. The two green arrows ought to be tip to tip in alignment.
There isn't a prayer of getting that joint back right with the ulna fracture left as it is. There isn't a prayer of holding that ulna fracture in the precise position with such a short span. This is a case for metal and luck. Both are needed.
Take calcium, right?
mmmm... shesssshhhh... nah... well sometimes, mostly not. Depending on where you live in this big world. Calcium is seldom an issue. Most healthy <the American diet is anything but that!> diets have an abundance of calcium - even an excess - which is OK. Children who do not drink milk clearly take longer to heal their fractures. In clinical practice, the first question when the expected healing isn't seen, is "Does s-he drink milk? The response is inevitably - Doesn't like it, or gets the snots if, or allergic to - whatever. But it isn't the calcium. It's the vitamin D. Cows don't put it there. Lab folks do. It is put in the milk. If children do not drink milk, fine, put the vitamin D in something else. But D stands for dangerous. Have the pediatrician tell you how and how much. D can be deadly if overdosed.
Children with seizure disorders can be very D deficient acting. We see this regularly . It isn't rare. The medications used to treat seizure disorder interfere with vitamin D metabolism. They can act deficient with normal intake. They need upward adjustments above the norm in many cases.
So recently, the pediatric gurus have finally caught up with we who treat fractures and bone graft and have conceded that the recommended vitamin D dosages were not optimum but borderline! So if you have not had this conversation with your physician since 2008, then revisit those requirements. However, you can overdose on Vitamin D, so don't go chugging the stuff.
Some Specifics
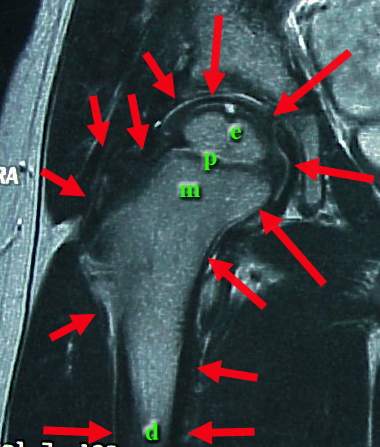 In this magnetic resonance image (MRI), which shows all kinds of tissue, we see the upper femur. The edges of this one bone are pointed out by red arrows. Within that
bone are zones - e,p,, and d.
In this magnetic resonance image (MRI), which shows all kinds of tissue, we see the upper femur. The edges of this one bone are pointed out by red arrows. Within that
bone are zones - e,p,, and d.
p=physis (growth plate). Cartilage looks black in this MRI. The physis is cartilage.
It adds length to the long bone. Above it (above= epi) is
e=epiphysis. The epiphysis is the growing joint end It grows radially.
m=metaphysis. The metaphysis ("next to" or "near" the physis) is the spongy bone near the physis which is made by the physis. As it matures, it thickens and
reorganizes to become the hard tubular bone shaft called the diaphysis.
d=diaphysis. (dia means away from). The dense bone tubular bone is also dark compared to the lighter color of the bone center which reflects bone marrow. Bone marrow is in the
epiphysis, metaphysis, and diaphysis.
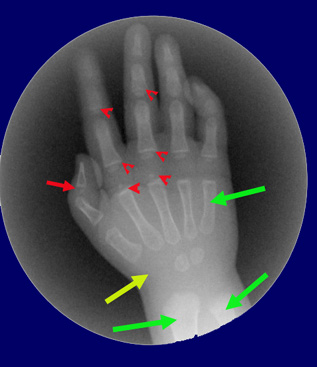
In the baby hand on the right we see the wrist area (yellow arrow) containing the short bones of the wrist. Two of the eight bones have begun to convert to bone material and have centers of bone which look roundish. Those bones are not round. Only the calcified centers show on x-ray unlike the MRI which shows the full structure.
The red arrow and arrow heads point out physes (growth plates). The green arrows point out long bones - a metacarpal, the radius and ulna.
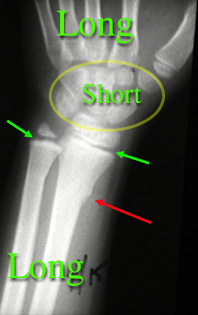 An x-ray from an older child who fell is on the right. Note the shapes of the short bones. The metacarpals are long bones, but have growth plates at only one end rather than both ends.
An x-ray from an older child who fell is on the right. Note the shapes of the short bones. The metacarpals are long bones, but have growth plates at only one end rather than both ends.
The radius has a toros fracture ( a buckle fracture) pointed out by a red arrow. The growth plate of the radius is NOT tender (same bone green arrow). However, the ulna bone is quite tender at the green arrow. Even though you can't see a fracture, we know that a small fracture exists in that ulna growth plate area. The reaction of healing seen on x-ray will often give it away later on.
The mix of bone types seen in this region allows us to determine where the individual is maturity-wise. We can tell that this girl is as mature as the average 7 1/2 year old ( called skeletal age 7 .5). The younger child above (round x -ray) is as mature as an average 1 1/2 year old girl.
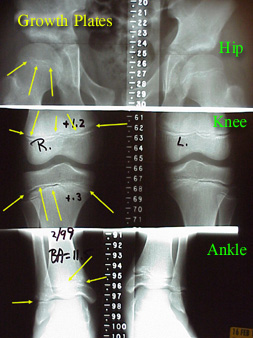 Here is one kind of scanogram, an x-ray with special technique and rulers to allow growth measurements. It shows the hips, knees, and ankles of a single youngster. The yellow arrows
point out the growth plates or physes (plural of physis).
Here is one kind of scanogram, an x-ray with special technique and rulers to allow growth measurements. It shows the hips, knees, and ankles of a single youngster. The yellow arrows
point out the growth plates or physes (plural of physis).
Notice that the shape of a growth plate isn't exactly flat but is unique to each joint. The odd or wavy shape of the growth plate helps stabilize the structure as cartilage isn't as strong as bone.
Failure of the growth plate at the hip is called Slipped Capital Femoral Epiphysis (SCFE). It can occur without trauma.
Trauma can cause failure at any physis...
 The knee, at the right, fractured through the distal growth plate of the femur. The proximal growth plate of the femur is at the hip end of the bone. The distal
growth plate of the femur is at the knee end.
The knee, at the right, fractured through the distal growth plate of the femur. The proximal growth plate of the femur is at the hip end of the bone. The distal
growth plate of the femur is at the knee end.
This fracture goes halfway across the growth plate then splits the metaphysis. The red arrows ought to be point to point and the green point to point. This is a bad fracture if the growth plate gets crushed in the process.

Here it is put back together. The growth plate did OK. But notice that the bump higher up is another entity (an osteochondroma) not related to this injury. It is common to find things on x-rays that are not related to the problem at hand. So we avoid attributing things to findings simply because they are there.
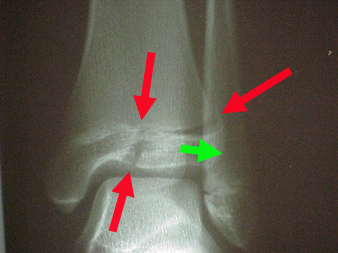 On the right we see an early teen ager. This fracture is almost unique to 12 to 14 year olds. The green arrow represents a ligament which attaches the fibula to the distal tibia epiphysis.
An outward twist pulls on the epiphysis. Because the growth plate closes from the inner side (medial) and the back side (posterior) first and from the outer front portion last - this anterior lateral chunk of epiphysis can
be pulled off from the rest (which is strongly anchored to metaphyseal bone where the plate has closed). The red arrows show the right angle path of the fracture through the growth plate and then into the ankle joint
by pulling the epiphysis apart. This needs to be put exactly back and fixed with pins or lag screw.
On the right we see an early teen ager. This fracture is almost unique to 12 to 14 year olds. The green arrow represents a ligament which attaches the fibula to the distal tibia epiphysis.
An outward twist pulls on the epiphysis. Because the growth plate closes from the inner side (medial) and the back side (posterior) first and from the outer front portion last - this anterior lateral chunk of epiphysis can
be pulled off from the rest (which is strongly anchored to metaphyseal bone where the plate has closed). The red arrows show the right angle path of the fracture through the growth plate and then into the ankle joint
by pulling the epiphysis apart. This needs to be put exactly back and fixed with pins or lag screw.
 This more mature adolescent has closed growth plates and is no longer growing at the ankle area. An ankle twist finds no weak spot at a growth plate and so fractures much like an adult right
through bone.
This more mature adolescent has closed growth plates and is no longer growing at the ankle area. An ankle twist finds no weak spot at a growth plate and so fractures much like an adult right
through bone.
 Here is a very visual example of another truism. X-rays may look OK but reality might not. The middle finger fracture is barely discernible on x-ray. It is read as
"non displaced" and as ""non angulated".".
Here is a very visual example of another truism. X-rays may look OK but reality might not. The middle finger fracture is barely discernible on x-ray. It is read as
"non displaced" and as ""non angulated".".
Normally, gently clenched fingers converge at a point near the "heel of the thumb". That the middle finger is aiming elsewhere means that the fracture is "malrotated". Malrotation is VERY difficult to see on x-rays - ever. There is no substitute for eyeballs in determining fracture position. X-rays are fine, but can mislead. Splinting a finger straight out (on a tongue blade) will fail to discover this malposition unless one is very attuned to the finger nail rotation.
PREVENTION!!!!!
This is a book in itself, most of it obvious (use the pads, the helmets, the face and teeth guards etc.). What isn't obvious and where kids, older ones especially, and adults just plain get broad-sided, is standing waves.
Huh? When you pluck a string a vibration makes it go up and down. But there are places that seem to be still. Harmonics. Divide the string in half and THAT spot is a 'node' a point around which vibration seems to center. Thirds, fourths. Music is based on this. Not so obvious is that if a kid is on one side of that node and the other side gets plucked, then the kid vibrates as much as if being directly on the spot plucked. It's like a see-saw, pound this end down and the other end goes up.
|
|
See? A kid on one side of a trampoline can launch a smaller kid on the other side into a dangerous situation.
The other thing is that padding prevents bruises but is a better weapon in that padded kids have no fear nor hesitation in running full speed into a brick wall. Only it isn't a brick wall, it's another padded kid whose knee gets ripped apart by the padded force that rockets into it as the foot is nicely spiked into the dirt guaranteeing no safe sliding outlet for that energy. That's how you break boards. Prop'em, whack'em in the middle. Pad them so you can really whack them.
Padding does change the behavior of falling. One is far more likely to lead with a shield than a bare hand. So elbow padding alters what is presented to the ground.
You may wish to look at our bone library
for bone by bone information.
There is so much more and exceptions are common. The main point is that there are many things to
be considered in treatment of children with fractures.