
There are types of scoliosis, but let us start off with some generalities common to most of them.
Scoliosis is not just any curvature of the spine. As seen from the side, the healthy spine is normally curved. The spine looks straight only when seen from the back.
Even so, small sideways curvatures are common and of no medical significance. Only when spinal curvature becomes a PROCESS, that is, when spinal curvature becomes exaggerated progressively - over time - do we apply the term "scoliosis".
The "curve" of scoliosis can be measured in several ways.
The most commonly quoted measure is the number of "degrees". If the vertebrae are stacked as blocks, then the
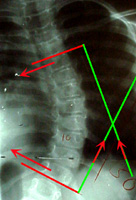 top & bottom vertebrae surfaces are parallel (with no angle between them). If the stack bends, then the surface of one block will project an angle to
others. The angle which is the largest (least parallel) is the measure used. Using perpendiculars to these lines (green lines on the right) is easier because the intersection of perpendicular lines can be kept on
the x-ray. It gives the same angle. Another measure is a count of how many vertebrae are in the referenced curve. You can have a 30 degree curve of 2 vertebrae or 4 vertebrae or 6 or 11, whatever.
Another measure is horizontal rotation, discussed below. It is mentioned least, because it measures poorly on an x-ray. It is not unimportant, however. Published data and
prognostication statistics are conspicuously silent on this horizontal component because of the inability to gather data of this kind from charts. The nasty deformation you see, is however, mostly this horizontal rotation.
top & bottom vertebrae surfaces are parallel (with no angle between them). If the stack bends, then the surface of one block will project an angle to
others. The angle which is the largest (least parallel) is the measure used. Using perpendiculars to these lines (green lines on the right) is easier because the intersection of perpendicular lines can be kept on
the x-ray. It gives the same angle. Another measure is a count of how many vertebrae are in the referenced curve. You can have a 30 degree curve of 2 vertebrae or 4 vertebrae or 6 or 11, whatever.
Another measure is horizontal rotation, discussed below. It is mentioned least, because it measures poorly on an x-ray. It is not unimportant, however. Published data and
prognostication statistics are conspicuously silent on this horizontal component because of the inability to gather data of this kind from charts. The nasty deformation you see, is however, mostly this horizontal rotation.
Let's go with what we can measure, first. Given only a single x-ray, we can only draw on statistics and certain clues to tell us whether a spinal curvature deserves to be called "scoliosis". Giving it a name implies something out of the ordinary. We know that in a growing youngster with no other problems, curves of less than 15 degrees do not have much more statistical chance of worsening (becoming progressively more bent) than a straight spine. But, over 15 degrees, the likelihood of curve progression does become greater. The more degrees of curve at younger age, the bigger the problem.
School Screening #/1000 kids 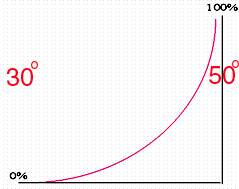
 Risk of Progression @ Maturity
Risk of Progression @ Maturity
<=Many growing children have curves of 15 degrees or less.
The % risk of late progression (in someone done growing) is seen on the right.
Note the landmarks in the data. Below 15 degrees is low statistical risk (even more true, the older the patient). Over 30 degrees, maybe, just maybe, things could sour. Fifty degrees is guaranteed trouble. Add to this, a bracing fact, curves of 45 degrees or more are very hard to hold. From these few facts you can almost deduce everything else.
We know this much, in the absence of any other factors, a girl (statistics are biased toward girls because scoliosis is by far more common in girls) with a curve of 30 degrees at the end of her growth MIGHT have a continued worsening of the curve even though she is no longer growing. It might happen, but it is not likely. With spinal curves of less than 30 degrees, it is very very rare to see scoliosis progression in the absence of other factors.
Between 30 and 50 degrees, the risk becomes real. At 50 degrees of spinal curvature, the scoliosis WILL progress, growth or not. Absolute. The medical objective is,
therefore, to strive to keep a spinal curve below 30 degrees until growth is completed.
This 30 degree curvature refers to an unbraced spine. Following bracing, once braces
are discarded, there is a certain amount of regression to the original curve measurement. The longer the brace is worn, the less the regression. Think of the spine as a sapling. If
you bend it, it springs back when you let go. But if it grows for a few years while held in a certain shape, then that shape becomes a final shape. Braces hold a shape, but GROWTH fixes that shape into permanence.
A brace applied late, near maturation, will not achieve a permanent result. The spine will behave as the wood of an archer's bow. It will yield to the brace but then spring back to its inherent curve when released. For this reason, JUVENILE scoliosis (scoliosis with no other medical cause attached, and 9 years old or less) has a much better brace cure rate. Young children are easier to straighten as they are more flexible, and they have more growth remaining to make a braced correction permanent.
Treatment - Overview:
A brace is used with curves measuring as low as 15 degrees if there are additional medical issues such as strong family incidence of curves with bad progression, or the presence of characteristics of the bone and posture on x-ray that seem to further dispose toward trouble. Wedging of vertebra (unsquare, trapezoidal) is an example. Absent that, no brace is used but the patient is monitored.
A curve of 20 degrees in a growing individual has a high enough chance of further progression and is close enough to the danger point of 30 degrees to warrant brace treatment with no further ado.
Why? Well, if you get to 30 degrees, you have no safety margin - curves above 30 degrees might progress, even after growth has finished. All it takes is one hot month in summer and a series of skipped wearings to wind up in the range of curvature that might progress at maturity. Take note that there are many reports on ineffectiveness of braces for scoliosis. They all come from hot places. Braces not worn do little.
Braces that attack the mechanics of curvature effectively do work. The problem is that there is much fluff out there regarding what a good brace is. Typically a "good brace" is "our brace" and a bad one is everybody else's. Sadly, that formula is seen again and again, both in private and academic medicine.
Let's be real. A brace that eases on comfortably, that leaves no marks, that "just holds the line" will fail miserably. Surgeons who use such braces will do a whole lot of surgery. But braces that squeeze the juices out of the patient and which attempt to use one formula (the So&So way) for every curve will also fail. Those braces wind up in closets if not in dumpsters.
Getting our facts right: in scoliosis, the spine does NOT just bend sideways. It also rotates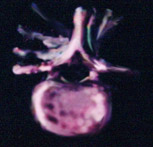 horizontally. It does not measure well on x-ray. Neither does intelligence. X-ray
is, well, x-ray, not an oracle. The model above shows the horizontal rotation trait. Marker sticks are drilled into the vertebral bodies parallel with the disk spaces. The sticks ought to be parallel. Both of the right images are "side" views. We ought not even see the sticks in these views. The tilt or "curve" as
measured on x-ray is the angle seen, in the left images, between the two marker sticks. That angle measured with a protractor is the curve measure.
horizontally. It does not measure well on x-ray. Neither does intelligence. X-ray
is, well, x-ray, not an oracle. The model above shows the horizontal rotation trait. Marker sticks are drilled into the vertebral bodies parallel with the disk spaces. The sticks ought to be parallel. Both of the right images are "side" views. We ought not even see the sticks in these views. The tilt or "curve" as
measured on x-ray is the angle seen, in the left images, between the two marker sticks. That angle measured with a protractor is the curve measure.
But look closer. The vertebrae have also rotated horizontally. Whereas the uppermost spine is facing forward, the vertebrae at the middle of the curve are facing toward the
right. Below the spine faces forward again. Braces must derotate segmentally to be effective. The shoulder girdle makes access to the uppermost spinal area difficult. Thus braces are least effective high up.
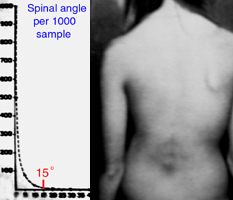
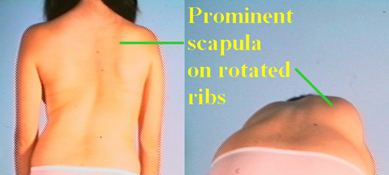 The effect of the horizontal rotation is seen best on forward bending. Notice that the "hump" is not the spine but rather right ribs that have been rotated backward. A left breast will seem to be larger as
the left ribs are as rotated forward as the right ribs are rotated back.
The effect of the horizontal rotation is seen best on forward bending. Notice that the "hump" is not the spine but rather right ribs that have been rotated backward. A left breast will seem to be larger as
the left ribs are as rotated forward as the right ribs are rotated back.
This girl is also  out of balance. Notice that the space between the left arm and the body is greater than the opposite side due to curvature, yet the
right arm hangs away from the hips while the left arm overlaps the hips due to shift - or "imbalance".
out of balance. Notice that the space between the left arm and the body is greater than the opposite side due to curvature, yet the
right arm hangs away from the hips while the left arm overlaps the hips due to shift - or "imbalance".
Small curve measurements can sometimes be seen with disfiguring rib rotations and side shifts. The "curve" angle
only measures a single facet of the problem.
The wing bone - scapula - sitting on the backward protruding ribs may "wing out". The severe hump, shown here, is the right rib cage not only rotated backward but sharpened
by the deformation of those ribs. They begin to fold into sharp rib shape angulation.
 |
Treatment - Bracing:
T he first brace of note was the Milwaukee. It has a nasty reputation. It was a beast, for
sure, running from jaw to hips, stretching as well as pushing. However, it was designed not as a conservative brace but as a substitute for a post spinal surgery total body cast - Oy!
he first brace of note was the Milwaukee. It has a nasty reputation. It was a beast, for
sure, running from jaw to hips, stretching as well as pushing. However, it was designed not as a conservative brace but as a substitute for a post spinal surgery total body cast - Oy!
Later, it was used to prevent surgery. It works. But it also fails many who could be treated effectively simply due to the inability of many youngsters to bear it. To wear it for 6 months post op is one thing, to wear it for indefinite years is another.
Lower profile braces were a response to this fact and to the fact that even the Milwaukee did not do so well for curves high on the spine (those just below the neck). For little benefit, the extra grief wasn't worth it. Incidentally, high curves have a lower percentage of progression, anyway.
A variety of lower - below the collar bone - braces followed. These were typically of unit construction from plaster casts taken of the patient. That cast, taken while pressure is applied to straighten the spine, determined how severe was the resulting brace pressure. If it was gently wrapped on and removed, you got a "mold and hold" brace. If the cast was made while the patient was pushed and twisted straighter, you got a "corrective" brace. They look similar. Some brace makers modified the castings to enhance the correction that would be applied.
Custom bracing is expensive.  A
A long comes some Canadian orthotists to Boston. The
state of Massachusetts was behind on orthotic payments for custom braces by eight years, leaving many orthotists bankrupt from huge unreimbursed outlays of time and materials. In that milieu, an idea
developed to mass produce a prefab series of braces, which would be modeled on girls without scoliosis. There were initially six such girls selected as models who were most like the body types of girls
long comes some Canadian orthotists to Boston. The
state of Massachusetts was behind on orthotic payments for custom braces by eight years, leaving many orthotists bankrupt from huge unreimbursed outlays of time and materials. In that milieu, an idea
developed to mass produce a prefab series of braces, which would be modeled on girls without scoliosis. There were initially six such girls selected as models who were most like the body types of girls  seen clinically. Later, more were added.
seen clinically. Later, more were added.
With the Boston brace, a stock item (like shoes), best-fit brace was worn. The brace would be cut away in areas where the orthotist wanted the anatomy to shift. It was effective for curves from mid thorax down. As none of the alternative braces were of much effectiveness in higher curves, this seemed to be the brace to beat. One problem, the absolute snug fit makes it hot. It works in Boston better than in Dallas. A second problem is discussed later.
Attempts to capture higher curves but still use the Boston prefab led to hybrids such as the Milwaukee-Boston. The jaw killer high neck piece was often dropped to a mere low necklace level (need some kind of ring up top to stabilize the metal uprights).
 The New York brace was a hybrid of old and new. It used the push and twist plaster cast methods of custom bracing and added inside pads that could push more or less at certain key
points. It was, and is, a highly effective brace but more difficult to fabricate and to sustain. This brace has many air spaces and holes. It is less onerous in heat. Theoretically, it
can push until it breaks something or gets it straight, but you can adjust it to tolerance. Too much zeal in applying corrective forces can lead to misery and that to disuse and thus to failure.
The New York brace was a hybrid of old and new. It used the push and twist plaster cast methods of custom bracing and added inside pads that could push more or less at certain key
points. It was, and is, a highly effective brace but more difficult to fabricate and to sustain. This brace has many air spaces and holes. It is less onerous in heat. Theoretically, it
can push until it breaks something or gets it straight, but you can adjust it to tolerance. Too much zeal in applying corrective forces can lead to misery and that to disuse and thus to failure.
That NY brace has dynamic pads as did the old Milwaukee. That's right, dynamic pads are NOT new. The Milwaukee dynamic  pads were limited by their central bar strap
suspension. The pads could behave better as pulling slings toward the left or toward the right, but not as horizontal twisting devices, ineffective at pushing forward or backward. The New
York brace can anchor a pad any way anywhere, and so twists as well as pushes. This brace has had heavy use since 1976. It takes a brace maker who really understands scoliosis to get it
right. The low bidder HMO official orthotist who slaps on some flexible prefab will certainly not get this brace right (nor change the progression of scoliosis).
pads were limited by their central bar strap
suspension. The pads could behave better as pulling slings toward the left or toward the right, but not as horizontal twisting devices, ineffective at pushing forward or backward. The New
York brace can anchor a pad any way anywhere, and so twists as well as pushes. This brace has had heavy use since 1976. It takes a brace maker who really understands scoliosis to get it
right. The low bidder HMO official orthotist who slaps on some flexible prefab will certainly not get this brace right (nor change the progression of scoliosis).
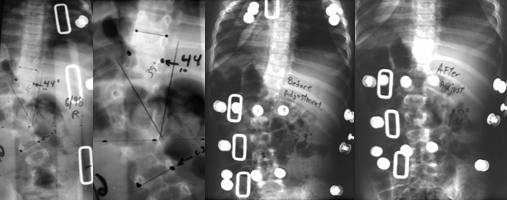
Below is an example of dynamic pad usage. A spine with a 44 degree curve in a "mold and hold" brace (second view is close up) is switched to a
dynamic brace. The initial wearing attains reduction of curvature to 29 degrees.
 |
A new variation on this theme replaces pads with air bladders. Sounds nice, but the forces applied by balloons are less directed. It is also hyped as the "only" dynamic brace for scoliosis. Maybe the only one on that fellow's block. Where's he been anyway?
The Charleston Brace: Charleston is a beautiful place. It is also warm and muggy. Who would be able to wear plastic on their body, there? Ah, but night and air conditioning allow another strategy. A Charleston brace is a very tall under arm brace which pushes you over so far that you can't even stand up, and can be worn only at night. You sleep in it. It is more corrective than a "day time" brace, but impossible to wear and walk in. It has a good track record for lower spinal curves, but not upper. But then, few braces do well with the upper. That it is a side leaning brace means that it is suited to single curves. Alas, many curves are not single but double (or S shaped) and others triple. There is no single solution for every problem.
The folks at Brown asked, 'Hey, why depend on the orthotist to get it right? Let a computer dictate where to push.' The Providence brace - a computer-guided mechanized brace in design and manufacture. Another city, another brace.
That's it? No. There is still a problem.
Common to nearly all the above, except some Milwaukee braces (only some), is abdominal compression. Children with neurologic disorders, often do miserably in any of the braces as mentioned. They are plagued by gastric reflux - compressing the abdomen can push stomach acid into the lungs. They do poorly with any squeeze to the chest or applied pressure against diaphragm movement. We get back to customizing braces again, but with this in mind and knowing what was learned from previous braces.
 The Summit Brace:
The Summit Brace:
We prefer the New York brace as a starting point. We want to have the ability to put twisting points at any location, and not rely on squeezing. But, thin plastic only gets stability from a
continuous, solid, cylindrical shape. In order to avoid abdominal compression, g-tubes, Baclofen pumps, V.P. shunt tubing, etc., we need very large cutaway areas from the original brace. What
is left is by itself not stable; however, we twist steel through the plastic frame to allow generous windows that avoid abdominal compression and which allow specific points of rotation to be set.
These Summit braces vary in how much opening they have, and where openings are,
depending on the need and on the child's tolerance problems. There has to be forward and backward push points to derotate horizontally. The metal is not just structural, but springy. The tension can be set and relieved by parents
etc. Why do this? Children with neuromuscular disorders need more aggressive bracing yet tolerate braces less. We need to side step the difficult to tolerate pressure points,
such as abdominal compression, and go aggressively after the rest.
In some cases, we can add the Charleston concept of ipsilateral (one-side) high configuration to the Boston concept of contralateral (other side) cut away, because the steel supports allow it.
The brace is created on top of a plaster likeness of the patient's body, cast while the patient was manipulated as straight as tolerated. The plaster model is then further altered to increase correction, using judgment of the patient's tolerance. No trim or cutaway from the plaster figurine is allowed without adding a compensatory relief zone, ensuring that the resultant brace will retain the full volume of the patient's body. Once the major brace form is made, it is reinforced with steel to allow for large cut outs. Pads are then added, some of which are attached to plastic, some to steel outriggers. These will be used to increase correction over time beyond that which was obtainable at the casting.
Note in the picture above the semicircular steel which supports a floating derotation pad
. These braces are hard to make and difficult to sustain with growth. They are justified by the complex and troubled nature of the population who wears them; we have
frequently used them successfully after standard bracing has failed and surgery was the only other remaining option.

An even more forgiving brace for paralytic single curves is the Summit 3 Point brace, seen here on the left in a side view. It is just an
open window frame which embraces the right side or left. An opposite side sling pad pushes the body through the large window. The metal uprights can nudge flexion or extension while the
sling corrects the collapsing curve.
If even this is not tolerated, and surgery is looming but deemed ill timed, then in the
face of progression, tricks to reduce the force that need be applied by the brace are called upon. One such trick is paraspinal botulinum toxin counterparalysis. It is
most useful in spasticity. It does not eliminate braces but just makes bracing easier in those selected cases.
Treatment - Spinal Fusion:
Spinal fusion is an operation performed for severe spinal deformity. Two major
problems require fusion and explain why certain conditions must be met by bracing.
1) Scoliosis that progresses
despite brace wearing in a growing youth.
2) Scoliosis in which the curve magnitude is great enough to progress
even after growth is finished.
It is most often needed for patients with advanced idiopathic scoliosis. They are mostly
healthy adolescent girls who generate the bulk of hospital derived data. The generality is that scoliosis in an otherwise healthy youngster is unlikely to worsen later if the curve - out of the brace - stays below 30 degrees at maturity. Spinal maturity is at about 14y/o in girls, or more exactly 2 ½ years after the onset of menstrual periods. This is
much more variable in boys and is typically several years later.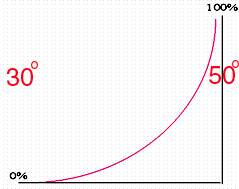
A curve of 50 degrees will always progress, even though all growth has ceased. We get a probability of progression curve that looks like the steeply curved graph shown here.
If a youngster has a curve that springs to above 50 degrees at the age of - say - 14, then there will never be a time that the brace could be discarded - nor will it
work. There is no point in bracing that curve. Most braces become more and more ineffective after 45 degrees, anyway.
With age past mid teens, the blood vessels change in how they supply the spinal bones.
Surgery in the young adult gets more difficult and loses more blood. You have to know when to fold.
SURGERY: FRONT OR BACK
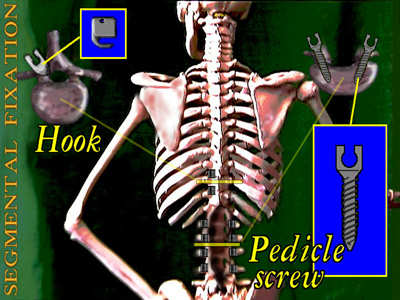 |
Above, in the upper left inset, we see a cross section of a single vertebra. The pointy upward process is the "spinous process". That is the bump you feel in the center of your back. One for each vertebra. You can see a roof over the spinal canal. The spinous process is the peak of that roof.
A hook can be placed against the edge of that roof to push upward or downward. A rod , spanning a length of spine with hooks at each end was used by Harrington to distract a curved spine straighter. This was a huge advance in scoliosis treatment.
Even so, you can only do so much with pulling the ends of a curve apart. You can no more totally straighten a spine by pulling from both ends than you can totally straighten a clothes line, with clothes hanging, by pulling on the ends. The rope will break first.
Correspondingly, the spine-hook junctions will fail. In fact, without successful bone
bonding (the individual bones joined together with more bone into one piece), that junction or the metal will fail eventu ally - always.
ally - always.
 The rod shown at the left in yellow is a Harrington-like rod with an upper and lower hook. At surgery it is jacked up until the spine is as straight as reason allows avoiding undo risks.
Also seen in the image is another device to be discussed later.
The rod shown at the left in yellow is a Harrington-like rod with an upper and lower hook. At surgery it is jacked up until the spine is as straight as reason allows avoiding undo risks.
Also seen in the image is another device to be discussed later.
A rod decreases the curve and betters the chances of fusion, as an attempt to fuse without rods once required total body casts and 6 to 9 months flat in bed. Even with this, a high number required revisit fusions because one area or another failed to fuse. The broken Harrington rod in the image on the right is not from bad metal (although the metallurgy today is much superior) but from the fact that a portion of the spine failed to fuse.
Over time, metal fatigues. We once had a patient come to us whose surgery, done elsewhere, seemed to have failed. When we took an x-ray we saw three parallel Harrington rods. Those surgeons were serious about avoiding failure. All three rods were broken. Without bone fusion, metal fails. Period.
From the back, the fusion is only that posterior roof surface. The larger body of the vertebra (the part shaped like a drum) in front of the spinal canal is unseen and untouched. Its growth might be inhibited if it is nearly at the end of growth, but that is less likely if the patient is young.
The two columns that connect the vertebra roof to the body are the pedicles. Screws might be placed inside those pedicles for various reasons. In spina bifida, wherein there is no roof over the spinal canal - as shown in the lower portion of the skeleton above -one might use such screws as there is no place to put hooks.
The older rods had one hook at each end. One pointed up and one pointed down. More modern rods are used in left-right pairs with multiple hooks along the length of spine to be fused. These hooks can pull sideways and pull a forward rotated side of the roof backward to correct the horizontal malrotation associated with the curve.
Such paired rods are far more corrective and thus depend less on pulling at the ends. There is more horizontal derotation and sideways pull than end distraction. This works much better. To stabilize the rods for such rotation, they are attached by metal cross links to each other as well as to the spine. Dr. Cotrel from France gets credit for this innovation. For industrial reasons an array of 'me-too' paired rod systems bear other names. They are essentially the same.
 |
Sublaminar wires (the roof segments are called lamina) grasp the roof parts using wires that are essentially twist ties. The ties are looped over a prebent rod. The holding power of this method is unexcelled. It was invented in Mexico by Professor Luque. The twist wires have the lowest profile of any device and thus tend to get used in very thin children who lack body fat, especially over the prominence of the mid thoracic area where hooks may raise bumps.
 |
However, the greatest correction ability comes from working on the less accessible body of the vertebra. The vertebra - boney drum shaped segments - are connected one above the other by flexible spacer discs. These discs are structurally like a jelly donut. There is a gel middle and a thick firm casing. [A ruptured disc is really only the jelly part leaking or pushing through the outer casing (the gel hardens as it hits the outside).]
In "anterior" surgery - the surgical incision is actually on the side so as to gain access to the vertebral bodies and full disk structures. This allows the entire disc donut to be removed, creating considerable space and flexibility, allowing much better corrective bending. Screws are inserted horizontally across the boney vertebrae, one across each vertebral body. A rod is placed through holes in the screw heads to hold the straightening.
Because the front resection of the entire disc complex also removes the vertebral body
growth tissue, the anterior growth of fused vertebrae is stopped entirely. Even when a good correction of curve can be obtained "from the back", in younger patients, the
crankshaft phenomenon caused by continued growth of the unfused vertebral bodies may upset that correction later. That alone urges 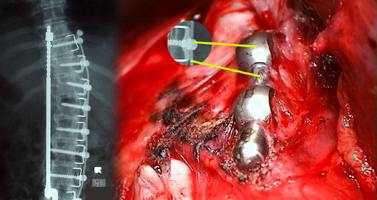 a frontal approach.
a frontal approach.
In the chest area, anterior spine surgery is performed from the side entering between the ribs. The anterior approach to spinal fusion first used a cable threaded through the screw heads, as seen on the left (rods came later). The cable system had a very low profile and still has use when space is very tight. It was the seed idea from which the various rod variations followed. Dr. Dwyer from Australia gets the credit.
 |
Anterior spinal rods are limited in the extent of spine that can be reached. Therefore long severe curves are corrected by first attacking the worst portion from the front and then fusing from the back over the longer span.
Because Luque wires are so versatile and derotate so well, they often are used along with hooks, especially in nasty curves.
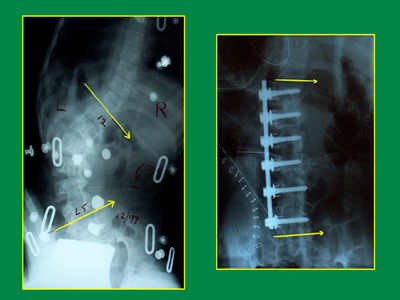
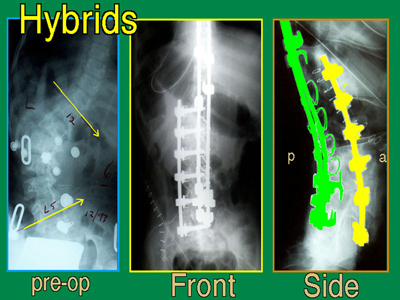
Here, below, is a hybrid that was used to treat a combination of paralytic scoliosis in combination with spondylolysis (when the spinal roof is detached from the vertebral body due to inborn reasons) creating an unstable lower spinal segment.
 |
Notice how the vertebral bodies are grasped from posterior by the "pedicle screws", as pedicle screws actually grasp the vertebral bodies in front by transversing the pedicles from the rear.
Pedicle Screws require spetial mention as the greatest forward momentum in surgical treatment is coming from the more extensive use of pedicle screws. The placement of pedicle screws is certainly more demanding. However, the ability to rotate, displace, compress or distract as well as hold difficult contours is becoming the role of pedicle screws. Anterior releases may forgo correction, leaving that to pedicle screws placed from the back. Much of this depends on the anatomy and what has come before.
Metal Bending:
Another technique which we developed for the very complex curves required special
metallurgy and instruments. In that technique, typically hybrid, the rods are affixed to the spine with the rods bent to match the complex of curves, uncorrected. Multiple
rotation and stabilizing points are temporarily set up for special metal bending equipment which corrects the metal curvature carrying the spine with it. This method
allows very complete disconnection of the vertebrae without worrying too much about things sliding around. It prevents sudden anything. It is best suited to triple and
quadruple curves where spinning implants is compromised.
Examples:
If the spine is fused from the back only (which does not fuse the vertebral bodies to each other, which are in the front) while there is still significant growth potential remaining, the spine can grow away from the metal in a twisting manner (as the vertebral bodies are in front of the spine). This is called "crankshaft" deformity. Crankshaft growth is nasty because the twist is happening in a post surgical spine with little place remaining to dissipate the distortion. It can be very unsightly.
 |
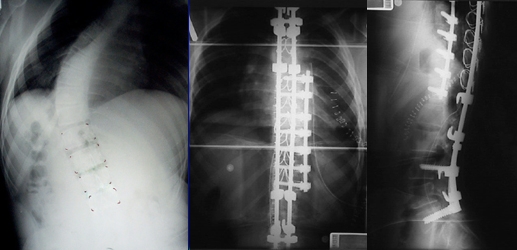
The boy above initially had scoliosis straightened surgically. He was described as straight post operatively. He had a posterior spinal fusion (not by us). Because he was not fused anteriorly as well, his vertebrae subsequently continued to grow (resulting in the above leftmost picture and x-ray). If the boy above had been a girl, growth may well have been near its end when this posterior spinal fusion was performed. The limited range of fusion did not stop the twisting crankshaft anterior growth from pivoting on the posteriorly-fused area and remaining spine.
To correct this deformity, we had to take down the old fusion (remove the fusion bone and uncover the buried metal), remove the metal, disconnect the vertebrae from one another at nine levels, close the back, then perform anterior spinal surgery from the front approach to undo the crankshaft, close that, and then return to the posterior spinal area - again - to reinstrument (new longer hardware) and set down new bone graft and close again (resulting in the above rightmost x-ray and picture). That is a lot of surgery!
Again, had he been older, the original surgery might have sufficed. But absent any success in holding the curve static in a brace until he got older with less growth potential, anterior surgery would have been more likely to hold.
Spinal surgery is complex in goals and techniques. We can't make you an expert in the nuances which vary with age, underlying other diagnoses, sex, vertical extent, curve angle, and horizontal rotation.
Some additional examples may help show the complexity:
example 1:
An advanced paralytic curve with severe imbalance in a patient with a shunt for
hydrocephalus complicating cerebral palsy (left x-ray). In this case, a high level of correction was obtained using anterior and posterior methods.
example 2:

A triple curve. The central curve drives the progression, but the top curve is stiff and does not yield to corrective forces. Straightening only the central curve would have the
patient leaning over, badly. To achieve satisfactory correction, the central curve was addressed anteriorly, then the entire complex of curves was stabilized posteriorly with a
degree of correction that would not have been possible with posterior-only methods.
example 3:

Same idea, except that the patient is older and the upper and lower curves are more supple. A hybrid (hooks and looping wires, and in situ metal bending) posterior system
does most of the job. Only small disc excisions from the front using a single small incision are needed. The metal was bent when placed, then straightened.
example 4:

Idiopathic curve, way out of balance, but supple above and below, stiff in the middle. Only the central part was operated from the front. Then the patient is followed to be
sure that the longer posterior construct won't be needed. Because the patient is older, he may very well not. It turned out that it did well as is. The patient wore a night brace
through the remainder of growth to help the odds.
example 5:
Scoliosis with an extremely rigid and advanced curve. Treated with hybrids.
Severe scoliosis and scoliosis with severe paralytic conditions behaves differently
and requires other considerations. You can read more about this is you wish (next button).
![]()
![]()


