|
The hard thing is knowing when to do what and how far to go. Motherly protective instincts tend to protect the status quo and may deprive a child from betterment. The overly zealous
approach may invite complications. The magical thinking tendency hops from one hocus pokus offering to another.
So how can we better our odds for improvement at each decisional step? First reduce risks by not chasing after ghosts. Not all FINDINGS
are PROBLEMS. Treat problems not findings.
Problems are those things which are known to damage anatomy or which reduce function.
Given a choice between two options, never trade on function. Words like stronger or straighter or more anatomic do NOT translate automatically into being more functional. When the neurologic condition is considered, a primary mechanism might not be functionally viable. Secondary mechanisms might be more reliable and attainable. Make decisions in view of a specific functional goal. One good way to select goals is to imagine the youngster grown up. What do you see now that would be intolerable later? Intolerable. That's not the same as wishful thinking which would have history rewritten. Selecting to intolerables tends to keep us grounded in both reality and practicality. We are not treating children. We are building adults.
Given an intervention plan, there are always two phases, attain and maintain. Seldom are the actions and strategies of maintaining our goal the same as those of attaining the goal. As a
generality, it is harder (takes more of something) to attain change than to maintain it. Therapeutic needs after an intervention may well be of lesser scope of force. The smaller scope of maintaining change
may seem less significant and thus be set aside. That's a mistake.
Do not treat exercise as religion. Do not have faith in exercise or any treatment method for that matter. Exercise must be judicious and monitored. Somehow any given malady regardless of
extent can be mentally erased by the word exercise. Exercises which repetatively coerce a resisting part depend on that resistance being weaker than everything else connected to it. If the forces are high, those
adjacent structures are more likely to deform in the process. If it feels as if you are pushing hard, you are. Use reason. When doing an exercise, ask what else
might happen. Look for it. Think of it this way. If stretching is supposed to be stretching the muscle-tendon unit and in fact it isn't, then something else is being crushed. We have witnessed crushed ankle bones following " aggressive " stretching exercises for equinus. The crushed extruded bone wound up pressing on nearby nerves which had to be surgically decompressed as if caught up in a tumor.
The forces required to attain a certain length or posture may well exceed tissue strength in many parts of the body. When using your hands always use your head.
Intervention in cerebral palsy is of several sorts:
* Prevention - to avoid known pitfalls
* Education
- overcoming perceptive learning obstacles
* Training - assistive tricks to attain motor skills
* Reconstruction
- undo physical damage which has occured
PREVENTION:
HIPS & KNEES :
The single biggest need is to prevent good hip sockets from going bad. X-rays are vital. We are quite blind in our hip exams. Hips have to be way gone before they feel bad to hands on examination. So, even with things going well, a single view of the pelvis that shows both hips is needed each year.
 What we do feel in examining the hips are tension and off-centering of
range as allowed by unbalanced tension. These are things which correlate with hips growing in an odd way. Early on, good x-rays do not mean
things are fine. Much of the hip outer structure is cartilage and not seen on x-ray. In the image on the left the orange shows hip structure not seen on
x-ray. This is the critical growing surface. The yellow shows the femur bone cartilage which is far larger than you would guess from the bone seen on x-ray. The hip can be
migrating with shallow structure and not appreciated as the bone portions do not reflect the damage until late. What we do feel in examining the hips are tension and off-centering of
range as allowed by unbalanced tension. These are things which correlate with hips growing in an odd way. Early on, good x-rays do not mean
things are fine. Much of the hip outer structure is cartilage and not seen on x-ray. In the image on the left the orange shows hip structure not seen on
x-ray. This is the critical growing surface. The yellow shows the femur bone cartilage which is far larger than you would guess from the bone seen on x-ray. The hip can be
migrating with shallow structure and not appreciated as the bone portions do not reflect the damage until late.
 If you only intervene when x-rays look off, then you
are waiting too long. The soft cartilage can be quite distorted before any bone changes are seen. As it is the cartilage which does the growing and sets the form for growth, cartilage distortion may then
translate to a permanent incorrect growth pattern. That is where the shallow vertical hip sockets primarily come from as the upper cartilage gets flattened upward then grows upward rather than outward. If you only intervene when x-rays look off, then you
are waiting too long. The soft cartilage can be quite distorted before any bone changes are seen. As it is the cartilage which does the growing and sets the form for growth, cartilage distortion may then
translate to a permanent incorrect growth pattern. That is where the shallow vertical hip sockets primarily come from as the upper cartilage gets flattened upward then grows upward rather than outward.
On the right is the outer surface of the left pelvis. Even in a more mature child, the edge is soft (shown in yellow tint) and more readily damaged by edge pressure.
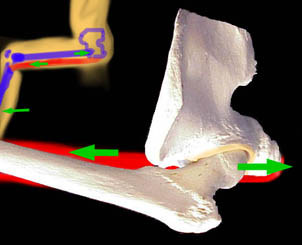 Y ou ought not direct strong forces against that soft growing hip edge cartilage in the process of doing exercise. For that reason, hamstring stretching ought
to be performed in an ABDUCTED posture. Above, with the hip flexed and adducted or at neutral, the ball of the femur is driven forcefully against the back wall of the socket and against the edge. In lesser
degrees of hip flexion the more superior edge gets the hit. The hamstrings, shown as red, connected to a long lever (tibia) with a 10:1 mechanical multiplying leverage can do real damage to the joint if the
hamstring fibrosis is tougher than the joint cartilage. Y ou ought not direct strong forces against that soft growing hip edge cartilage in the process of doing exercise. For that reason, hamstring stretching ought
to be performed in an ABDUCTED posture. Above, with the hip flexed and adducted or at neutral, the ball of the femur is driven forcefully against the back wall of the socket and against the edge. In lesser
degrees of hip flexion the more superior edge gets the hit. The hamstrings, shown as red, connected to a long lever (tibia) with a 10:1 mechanical multiplying leverage can do real damage to the joint if the
hamstring fibrosis is tougher than the joint cartilage.
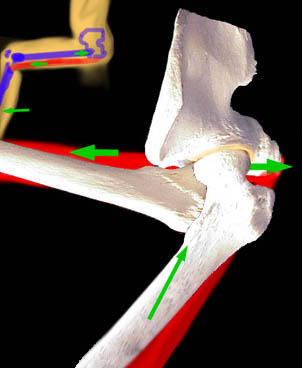 By abducting the hip when hamstrings are stretched, the forces are directed into the socket at center and
not against the soft edge. If there is an adduction contracture which sustains adduction, then hamstring stretching can be quite nasty on the hip socket. By abducting the hip when hamstrings are stretched, the forces are directed into the socket at center and
not against the soft edge. If there is an adduction contracture which sustains adduction, then hamstring stretching can be quite nasty on the hip socket.
It should be pointed out that the combination of hip adductor plus hamstring contracture is highly associated with development of hip dysplasia
(flattening and loss of socket stability) and vertical orientation.
ANTEVERSION:
But there is an additional issue. The direction of the knee is always called the zero point. We measure
from the knee. Below, the green line is a sort of mechanical axis of the knee (an approximation). Notice that the hip end of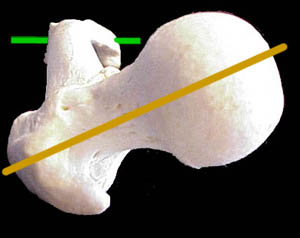 the femur (yellow) - the femoral neck and head - are not parallel to the knee axis. The
head is oriented about 30 degrees forward (forward= ante turned=verted) or 30 degrees anteversion. If the anteversion were, say, 70 degrees, then the femoral
head neck axis (yellow line) would be nearly vertical. With the knee pointing forward, a badly anteverted femur levers the ball with a twist out of the socket.
The knee has to point inward for the hip to center. the femur (yellow) - the femoral neck and head - are not parallel to the knee axis. The
head is oriented about 30 degrees forward (forward= ante turned=verted) or 30 degrees anteversion. If the anteversion were, say, 70 degrees, then the femoral
head neck axis (yellow line) would be nearly vertical. With the knee pointing forward, a badly anteverted femur levers the ball with a twist out of the socket.
The knee has to point inward for the hip to center.
 This problem is the basis for the varus DEROTATION surgery (derotation means get the anteversion corrected) or VRO. There is no exercise to correct
anteversion, as such. We do know that to become a ballerina, you need some retro-version (less than the anteversion shown here, where the yellow line is more parallel to the knee axis). To get to that condition
requires specific turning exercises from a very early age. Twelve is too old. Looking again at the yellow in the above hip x-ray we see that the soft cartilage of the upper femur over the head and neck area is what
allows this rotation. Once this cartilage is gone, the ability to rotate the bone is gone. Rotation of such a
bone requires repetitive muscle forces, the bone cartilage sufficient to the task and (the big one) a stable joint that won't pull apart instead. This problem is the basis for the varus DEROTATION surgery (derotation means get the anteversion corrected) or VRO. There is no exercise to correct
anteversion, as such. We do know that to become a ballerina, you need some retro-version (less than the anteversion shown here, where the yellow line is more parallel to the knee axis). To get to that condition
requires specific turning exercises from a very early age. Twelve is too old. Looking again at the yellow in the above hip x-ray we see that the soft cartilage of the upper femur over the head and neck area is what
allows this rotation. Once this cartilage is gone, the ability to rotate the bone is gone. Rotation of such a
bone requires repetitive muscle forces, the bone cartilage sufficient to the task and (the big one) a stable joint that won't pull apart instead.
If the socket isn't rock solid stable, then rotatory forces may damage the socket rather than nudge
rotation into the upper femur. How the leg is turned matters. There is a long history to dancers exercises. But they are based on an assumption of normal deep anatomy.
W-Sitting wherein the child sits on the floor between the feet with knees 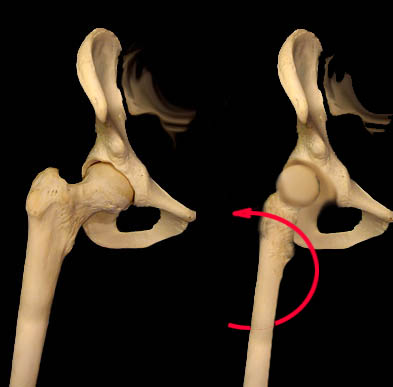 forward does several things. The ball of the femur is pressed very strongly against the inner wall of the
socket (which isn't going anywhere). That is a very unyielding force application to rotate the cartilaginous femoral neck (yellow in the image above). The femoral neck becomes anteverted relative to the knee over
time. forward does several things. The ball of the femur is pressed very strongly against the inner wall of the
socket (which isn't going anywhere). That is a very unyielding force application to rotate the cartilaginous femoral neck (yellow in the image above). The femoral neck becomes anteverted relative to the knee over
time.
Now when you point the knee forward (red arrow) as in standing or sitting that anteverted femoral head and neck twist out of the socket with high leverage.
So the inner wall of the socket is a
stable structure which can apply a strong resistance to the twisting femur. But, the reverse untwist so to speak is to unseat the ball out of the socket.
That is poorly resisted. Thus the W-sit has high forces to deform Once deformed, the socket gets attacked by the twisted deformity and then the socket fails. Thus the late dislocation. X-ray detects nearly
none of this until the socket is substantially compromised.
Lesson? Don't wait for x-ray changes to intervene in things we know can go bad and which are set up to go bad.
Such as? Hip adduction contracture or sustained high tension, especially in association with flexion will
eventually damage the hip joint. Obviously exercises to stretch the hip adductors are good. And remember that hamstrings are strong adductors as well. Include them. Then get real. Stretching exercise is
not "exercise", as in weight lifting. It is a pull being applied with substantial leverage to tissues. The thing that "stretches" or better stated which "gives" is the tissue most able to give.
When fibrosis in the muscle is very strong, it may be stronger than the joint cartilage which will give
instead or than mineral poor bone which may crack instead. "Hamstrings stretching exercises" CAN break femur bones or dislocate hips as well. Use reason. Ask, is this much force (which you feel with
your hands) really safe? Do I feel the springy give of muscle? Or am I hitting a wall? Know when to fold.
What other ways are there to get adductors or hamstrings to elongate with less risky force? Botox is
useful if the resistance to stretch is high and if the muscle does feel stretchy. Beware of fibrosis. Fibrosis is
like having a piano wire running through the muscle. It takes all the tension. Indeed, one of the reasons muscles can be felt to be weak after "lengthened" is that the unyielding fibrosis was taking all the force
and the muscle was doing nothing. A muscle may be both very weak AND very resistive to range (because of the fibrosis).
Botox will not soften anything if the main cause of resistance is fibrosis. Fibrosis is very much like scar.
Nearly identical, except that it does not require an overt injury to be there. It just forms. About the only thing that lengthens firm fibrosis is dividing it.
One half of all the surgery this author does is due to the effects of prolonged sitting. Sitting all day then
sleeping fetal posture at night will result in substantial shortening of muscles. Schools often want a doctor's note for exactly how long a child may be out of their chair. It ought to be the other way.
Prolonged sitting causes all sorts of problems, problems which lead to a high incidence of surgery and big operations at that.
Alternatives to sitting ought to be built into activities. Computers work just fine when the user is standing. We can still grasp the code of Hammurabi when we listen standing.
 Sitting ought to resemble sitting on a horse. Knees together or even thighs parallel is just awful for hips. See the Mary Chair. Sitting ought to resemble sitting on a horse. Knees together or even thighs parallel is just awful for hips. See the Mary Chair.
When knees are apart, in a chair, the ankles ought to be as wide apart and the feet should point outward (not straight ahead). The twist on the legs, caused by
pointing feet straight ahead, twists the knees and the hips.
SPINE : A child who leans to one side constantly may develop a growth anomaly which grows that way, paralytic scoliosis. Side supports, you would think
ought to prevent that. But they have to be very tall and very tight to do so. The reality is that winter and
summer clothing, being so different, make tight fitting side supports ineffective. If a child tends to lean to
her left, then raise the left side support high. Center the right support at the mid bend and push it way in.
Keep the tush centered. Vertically offset side supports are far mor effective and allow clothing thickness to change.
 Beware of "truncal weakness". It might be just that. But very often what is called truncal weakness is actually hamstring tightness. The hams are very
powerful muscles and in a pelvic duel with abdominal muscles will win every time. The "weakness" may be simply relative. Sitting cat backed is, more
often than not, a sign of hamstring tightness backward tilting the pelvis. Beware of "truncal weakness". It might be just that. But very often what is called truncal weakness is actually hamstring tightness. The hams are very
powerful muscles and in a pelvic duel with abdominal muscles will win every time. The "weakness" may be simply relative. Sitting cat backed is, more
often than not, a sign of hamstring tightness backward tilting the pelvis.
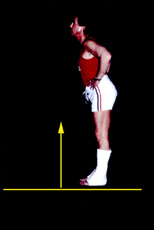
Another source of bogus truncal weakness is jack-knife posture due to tight calf muscles. Equinus tilts the shins backward and the body would fall over
backward if not for a balance reaction - flexing at the hips. Here, on the left, a normal volunteer placed into casts which are in "equinus" (toe down) can only
stand by hip flexion into jack knife posture. He has no truncal weakness nor hip contractures. To stand erect, the shins must normally - for all of us - forward lean by about 8 to 15 degrees. We call that functional dorsiflexion. So called "neutral position" is 90 degrees and is not functionally neutral. At 90 degrees (square) we fall
backward or have to jack knife for balance. To stand erect with so called "neutral" braces, requires a shoe heel which raises the brace heel and thus obtains the forward tilt of the shins required for relaxed
balanced stance.
ANKLES & FEET : Feet going into "valgus". Everted feet are very common in  CP and in any condition
where the "Achilles is tight". When people say the Achilles is tight that does not mean the tendon (alone) is tight. The entire motor unit muscle, myofascia, and
tendon are tight. They are all links in the same chain. CP and in any condition
where the "Achilles is tight". When people say the Achilles is tight that does not mean the tendon (alone) is tight. The entire motor unit muscle, myofascia, and
tendon are tight. They are all links in the same chain.
If the true ankle bone (talus) can't tilt up in front because the calf muscles with
Achilles tendon are holding the heel up in back, then the joint below the talus (subtalar) yields. That motion, below the talus, is on a trajectory looking like the
surface of a cone whose point is the tip of the heel (where the Achilles attaches, trajectory shown in green). So the Achilles attachment becomes a fixed pivot point as the subtalar joint slides laterally (outward) into what is called "valgus" posture. Valgus often gets called (groan) "pronation". [Just for the record there is NOTHING
pronated in such a "pronated foot", as the forefoot gets counter twisted into supination by staying with the floor as the heel rolls out.]
Whatever. Just know that although the foot can be pulled outward by specific muscle action of everting
muscles it can also be trapped or stuck there by secondary shortening of those same muscles after the everted posture is established by the primary cause. The primary cause is usually the "tight heel cord"or
"Achilles" or "gastrocnemius" or "calf muscles" or "triceps surae"... so many names for hunk of anatomy.
So, to prevent the rocker or pronated (bad word) foot is to maintain supple length of the calf musculature
to allow the talus or ankle bone true up down action and not call into play the lower subtalar outward rocker motion. That out rocker motion also exposes the talar head on the inner side of the foot showing
as a nasty and tender bump on the inner side of the foot near where the arch is supposed to be. To get rid of that bump the heel needs to be tucked back under the talus which in turn requires (given the Achilles
shortening) that the heel be in equinus which started this cycle in the first place.
To correct valgus, or pronation, or the inner foot bump requires getting the calf muscle out to length first.
What we say is that gastrocnemius or Achilles lengthening is permissive of correction. Foot posture correction then has to be held by some means. Often that means is a brace or shoe insert of some kind.
So then, if the everted foot is to be prevented calf muscle must be stretched. It must be kept stretched as
the child grows. Attain. Maintain. Serial casts might be used to attain the length. Maybe Botox on top of exercises when exercises are not going well. Or even braces used at night when things have gone well but
there is a long growth period remaining.
Do not stretch the calf or Achilles by pushing up on the forefoot near the toes. Chances are good you will
sublux the midfoot. You must keep the heel under the talus and stay away from the forefoot which will bend easier than the calf will stretch. Also remember that the calf muscle has three parts (hence one of the
names = triceps surae). Of those three portions, two of them (gastrocnemius) attach above the knee. If the knee is bent when the exercises are done then only 1 portion of the three part muscle is getting the
exercise. That happens to be the least likely portion of the three to get contracture, by the way.
Wearing AFOs at night is a great way to keep the calf muscles stretched out when daytime wearing
seems too much for functional needs. But braces are only good at maintaining stretch and less good at attaining stretch. Stretching with braces often simply hurts. Skin can take only seven pounds per square
inch pressure before breaking down. Also braces have maximum leverage at the forefoot where we least want to push.
Summertime camp is wonderful and in September we have a bunch of kids tight from a summer of bliss -
braceless bliss. Typically, such short lived tightening can be stretched out with a cast (or two) or a single
Botox shot to be followed by resumption of braces to maintain correction. All is not lost and the campfire stories are worth it.
EDUCATION & TRAINING : Suffice it to say that at birth, the scope of brain yet to be built is still quite impressive. Brain injury can repair, but it is variable. Function can be reassigned, more so the earlier
the deficit. But we have learned that the repair looks to ongoing function to get it right. Education is not just somebody blabbing and somebody else listening. We may have to work around learning or
perceptual deficits. Therapies are rich in tricks to convey when communication of want is impaired.
Some use a barrage of verbal cues, some use reflex cues (jab here and whoops reaction there gets the
ball rolling), or manual or tactile direct hands on puppet-like cueing or using strings and elastics to steady
and direct movement. All have great results with kids - different kids. Don't expect a totally deaf kid to do well with verbal cueing. Tactile defensive kids may rebel to being prodded. Theories are fine for
opening gambits, but, as in chess, you have to respond to the board.
RECONSTRUCTION : See the rest of this web site.
|