|
 There is a wide gap between the
definition of cerebral palsy and the actual usage. By definition, cerebral palsy is a non progressive injury to the brain (or its
development) at or near the time of birth. The idea of the definition is to set CP apart from progressive neurologic disorders. Fine. There is a wide gap between the
definition of cerebral palsy and the actual usage. By definition, cerebral palsy is a non progressive injury to the brain (or its
development) at or near the time of birth. The idea of the definition is to set CP apart from progressive neurologic disorders. Fine.
However, CP in practice, is any person who needs CP services. In any CP center will be kids who were near drowned, struck on the head, or having any of a variety of much later
neurologic insults. So, practically speaking,
take the "at or near" birth with more than a grain of salt. In fact, about 40% of persons called CP (it varies with the nature of
the center) have underlying metabolic or genetic traits linked to the development of CP.
Another misconception is that the disorder is one of paralysis.
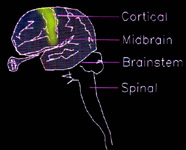
The name was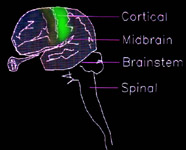 originally derived to emphasize motor skills and
thus remove the stigma of other names. In the above left picture the motor strip of the brain, if discretely injured, would fit
the bill. However, that is a fairly rare case. Injury to the sensory portion of the brain
is quite likely as well. originally derived to emphasize motor skills and
thus remove the stigma of other names. In the above left picture the motor strip of the brain, if discretely injured, would fit
the bill. However, that is a fairly rare case. Injury to the sensory portion of the brain
is quite likely as well.
Injury does not color within the lines, so to speak. A single injury may cross several zones of unrelated functionality, as the
scatter of orange, above.
We use the term "syndrome" to group oddly related traits that do not seem necessarily logically related. They become logical
by way of knowing the anatomy of the brain - or perhaps - the chemistry - or better - both.
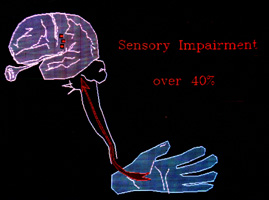 In fact, in hemiplegia, which is essentially a stroke, there is significant disability from the sensory loss in over 40% of
patients. For the leg, that may be a subtlety. The leg definitely uses sensation but isn't a sensory tool primarily. Stiffness + opposite leg cues (inference) allow fairly good substitutive mechanisms for
the key function, support and walking/stepping. In fact, in hemiplegia, which is essentially a stroke, there is significant disability from the sensory loss in over 40% of
patients. For the leg, that may be a subtlety. The leg definitely uses sensation but isn't a sensory tool primarily. Stiffness + opposite leg cues (inference) allow fairly good substitutive mechanisms for
the key function, support and walking/stepping.
The hand, however, is essentially a sensory device. Loss of sensorium in the hand is akin to loss of the hand itself, functionally. There are different kinds of sensation. Let us just
mention the biggies:
1) Touch 2) Temperature 3) Vibratory 4) Pain
5) Position 6) Movement 7) Spatial...
There's more. But from a practical perspective, use of the
hand depends on, and is in proportion to, the ability to discriminate. Examples include knowing a dime from a nickel by feeling the edges, a paper clip from a safety pin,
letters drawn in the hand such as W N T X O C with better than random score, telling burlap from silk, which side of a paper nail file is which , and distinguishing a warmed spoon from a cooled spoon.
We can nicely alter the shape of the hand, but if sensory testing goes poorly we are certain that such reconstructive measures will be primarily for esthetics, as the changes we
make will not be used. For hands, we can actually group our interventions as aimed at one or more of three functions : Grasp, Release, and Delivery.
Grasp - what it says, closing and holding onto an object
Release - letting go
Delivery - getting the hand to and oriented for grasp &| release
When trying to communicate your own observations, as to hand disability, you will do well if you group your observations into the above three areas.
Brain Injury:
Although actual clinical disease nearly never falls within pure anatomic boundaries, we 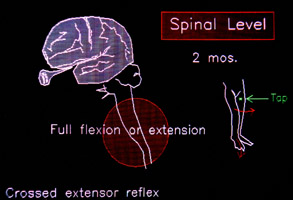 still need to know what the relative contributions are to the mix of pathologies. still need to know what the relative contributions are to the mix of pathologies.
The spinal cord is NOT just a conduit from the brain. It is rich in patterned associations between
movement types. In fact, the whole of walking motion, resides in the spinal cord. These patterns are set up as if X, then, most likely Y - and get ready in case of Z. These anticipatory helper
circuits are set up in utero by 2 months gestation. The brain does not dictate every nuance of movement, but plays the cord and embellishes the basics contained within the cord, or suppresses. Why? Probably speed. Nerve conduction is a wave of sodium/potassium interchanges, rapid, but not awesomely swift. The amount of information sent is far less if the main strategies are known at the periphery. Think of Scottish troops responding to the Great Highland Pipes at great distance. They
know what to do and don't wait to be told every detail.
Motor signals contain two components 1. do a certain thing and 2. expect that it will result or feel a
certain way. If the result does not match expectation, then it is handled on the spot by the local troops (reflex).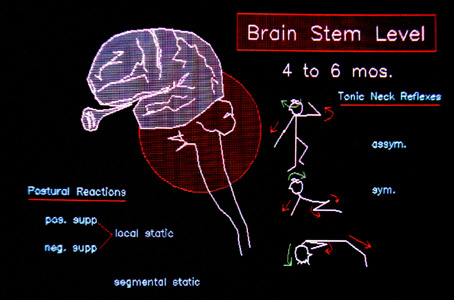
The brain stem, is the next organizational level above the spinal cord. It has even more complex patterns of stock movement it can call upon or deliver in
different levels of amplitude. As such, these patterns may superimpose on other finer actions so as to support them in a larger context. The most prominent of these are those bodily
tone shifts which accompany neck position. The asymmetric (looking right or left) and the symmetric
(looking upward or downward) have characteristic sequella. You may see children using neck posture to induce leg position. The strong urge to look down with stepping may be to see (sensory need) or
may be to enhance leg extension (neck reflex), or both. These movement associations are hard wired in the developing brain stem by about six months.
 The mid brain possesses additional movement modifiers. These include reflexes that assist righting
the body and draw upon orientation from the ears and eyes. Sitting without help requires these contributions. Alternating movements, called amphibian, as are used in crawling, come from here. Such neurologic
interconnections develop at about the intrauterine month number six. The mid brain possesses additional movement modifiers. These include reflexes that assist righting
the body and draw upon orientation from the ears and eyes. Sitting without help requires these contributions. Alternating movements, called amphibian, as are used in crawling, come from here. Such neurologic
interconnections develop at about the intrauterine month number six.
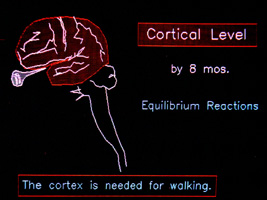
The higher functions, which we call cortical, come into being at about 8 months gestation (near the launch). They not only add to the complex of skills needed for upright equilibrium, but also are essential for walking. Real walking is not just a
sequence of left right left right left..., there has to be judgment, anticipation, fine control, initiation, and so much more.
Fortunately, in many brain injuries, the actual impairments do
not damage the critical cortical functions needed to walk. How can you tell? Hard to describe it, but there are certain "moves". The key element to the "moves" is speed. Speed of recognition of change, and speed of response. A child who is all twisted
may fail at walking but may seem to do well if supported a certain way. Change that way - quickly - and see if the child responds quickly such that had the response been of sufficient
amplitude, it might have worked. In other words, the response may fail because the scope of response is too small. We can deal with that. What we have no remedy for, is sluggish response or incorrect response. If a sudden change only elicits
a "yowie" or startle response not directed mechanically at the cause, then it is unlikely that any range of response can be turned into effective movement.
Another thing about the "moves", is where they are. Children who seem discombobulated in a standing posture may creep on all fours with apparent grace and agility. That is, there are control arcs, but they might not be stacked vertically. Control may be good but only through a narrow range. You do not want
more range of motion than the arc of control, otherwise, motion is uncontrolled. Uncontrolled motion is called falling. See walking.
Damage is not all or nothing. Even within a single muscle, we find abnormal activity and normal activity. When we see the
"moves", we see the process of walking control responding quickly and very often in a compensatory way (which might
look abnormal). However, we also see the superimposed pathology thwarting effectiveness. Another way of describing the "moves", especially in kids with spastic diplegia
(prematurity related, associated with PVL -later), is spasticity in parallel. One gets a strong sense of a duct taped normalcy.
There is quick and deft response working within other superimposed restraints (can run tippy toes but not walk without holding something, can tall crawl or walk upright on
knees). The key to the oddities is the answer to the question, "If I were that constrained, would I do that well?"
The other circumstance is spasticity in series. This latter kind of
function is slow and labored. Movements are carried out by the tone mechanisms or recruited mass actions, or bursts that
follow delay. The individual is using spastic patterns or rigidity patterns to perform the movements. These kinds of movement can not utilize momentum. Upright strategy becomes stepping, not walking (see walking) if momentum is not a part of the strategy.
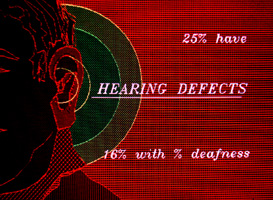 Because hearing is represented on both sides of the brain,
complete deafness is unusual (16% with some degree). Varied hearing defects, which include the interpretive aspects of hearing, are found in about 25% of patients. This varies between
clinics (because of the services offered). Because hearing is represented on both sides of the brain,
complete deafness is unusual (16% with some degree). Varied hearing defects, which include the interpretive aspects of hearing, are found in about 25% of patients. This varies between
clinics (because of the services offered).
Children may hear fine and understand what they hear but may have damage to those neural paths that allow word sounds to
be created. Alternate paths may solve this, hence sign language.
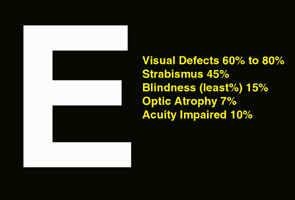 Our very advanced use of and need for vision makes visual disturbance a bigger problem. Vision is not generalized to both sides of the brain, but rather mapped. That mapping means we can have holes in
vision - blind spots, blind sides, or tunnel vision - as well as complete blindness. The binocular aspects also require coordination of very high precision in the muscles of the eyes. Our very advanced use of and need for vision makes visual disturbance a bigger problem. Vision is not generalized to both sides of the brain, but rather mapped. That mapping means we can have holes in
vision - blind spots, blind sides, or tunnel vision - as well as complete blindness. The binocular aspects also require coordination of very high precision in the muscles of the eyes.
Aspects of CP:
Depending on where the injury is, we know that certain functions may be absent. However, there may also be extras as well. An obvious extra, is seizure activity. Nerve cells look like
trees. The nerve cell has many branches which touch many other nerve cells. Some branches connect right back to the source (self stimulating) or connect to others which connect
back to the source. The idea is to keep a certain pathway of function active as long as some minimal requirement of new input keeps coming.
That input, alone, would not drive the system - as it takes several stimuli together to make the next neuron in line active. Most neuron loops also have shut-down neurons, whose action
inhibits. However, if damage creates a loop which lacks a such a dampening mechanism, then the loop can just keep going in circles. That activity constancy might even recruit additional
other loops by the mere constancy and increased speed of recycling. How far that goes determines whether a seizure (that's the name for it) is focal, or generalized. Where the
process is, that is, in what functional part of the brain, determines how that activity is perceived.
The same basic kind of recycling defect may in one place show up as a facial twitch, in another place in the brain - be heard, as
a buzz, in another brain location - cause a smell to be detected, in yet another - cause vomiting, or cause old memories to spring up, perhaps - cause concentration to fail, or cause
anything within the realm of neurologic function. Drugs which inhibit one kind of chemical transmitter or another or which slow the actual transit of the nerve impulse (thus depress such
looping) are called anti seizure drugs. They have many sorts of mechanisms of action.
A lack of sufficient inhibition in the spinal associative neurons (the "internuncial cells") allows them to over cycle and recruit
additional spinal circuits. This is spasticity.
If outflow comes from higher centers, such as exist in the mid brain, then more complex extras appear. They appear as
stiffness of limbs which alters with the position of the joints, near or distant. We may see waves of alternating joint flexion and extension such that one joint goes up, the next down, the
next up. Such dystonic postures are very much influenced by incoming stimuli - stimuli from any of the categories.
Stimuli are important and can be internal. A child with CP may
be suddenly posturing a left arm in a way not seen before. Chances are the stimulus has nothing to do with that arm. You may find a tooth cavity, or a sunusitis, or even esophageal
burning from reflux at the root of it.
Sudden severe leg posturing very commonly means bladder infection. Also look for splinters, thumb tack in shoe, anything..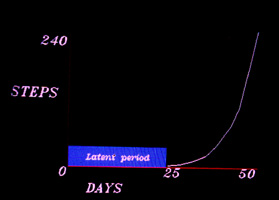
Early Evidence:
Probably one of the most
watched for of milestones is the onset of walking. Children may walk before 1 year or as late as 18 months with no difference between them in ultimate skills.
A child who takes first steps at 11 months might still wind up having an impairment. A better indicator of trouble is the lag time from the first step or two to free walking. If we graph the
number of steps taken (Y axis) against the days lapsed (X axis) we get this graph. A child who takes a step or two, but then 50 days later is still only taking a step or two, may well have a
problem, even if that child is only 14 months of age.
We do not expect to see handedness before two years of age. A one year old with a strong right handedness actually has left deficit.
Walking on toes is common early on. Yet, most kids do not stay on toe. Those that do, might also have another common
condition, congenital tight Achilles. This condition acts as a dominant inheritance. It can be very mild and subtle, and wind up being misinterpreted as cerebral palsy. It isn't. It is easy to fix.
Very young children with dislocating knee caps or hips will walk very oddly and often be confused as being kids with CP. It is important to check the hips with x-ray even when there is no suspicion by exam.
Orthopedic treatment falls into several strategies,
1) undoing after effects
2) reduction of active abnormal features
3) replacing what is missing
4) enhancing control mechanisms.
Any one of the above four strategies is an  advanced course in itself. Suffice it to say that all four are needed and often advanced course in itself. Suffice it to say that all four are needed and often
in combination. Least covered in this overview are the most spectacular procedures (as they are beyond what short discussion can convey). In a game that cannot be won, muscle transfers change the rules.
They act in all four strategic areas.
There are so many details and complicating issues. Facts in isolation can confuse. There are many treatments being hailed
and dangled before a population that will grab at any hope. Against that, there are the dogmatists who only accept what has been double blind proven and revalidated (and which is,
therefore, about 15 to 20 years old, if you are lucky). There are the inflexible academics who want to make every child a randomized subject. There are gait lab enthusiasts who think
that only machines dispense truths. The cookie cutter folks have an X for a Y, "The way we do it here...". You have to be flexible, as the variation is huge. Show me any study that
uniformly applies a specific single treatment over a large population of CP kids and I will show you a population with missed opportunities.
We do not have any magic advice here, except this: If the
words offered you sound fuzzy and vague then take the reasoning to be as well. In any decision, given a choice between function and something else, take function. When you
ask how to get there, also ask how to get back.
Getting REAL
Wasn't all that stuff above so ---mmmm--- organized? You just know a scholar who eats, lives, and breathes categorization did
that. Our real problem is that treatment chokes on that sort of grouping according to similarity of concept. The anatomy just doesn't fall out that way. Yes, lab experiments can create nice
squared off zones of injury. Yes, look hard enough and some case will fit. But most do not. The brain is seldom injured by a transverse cut.
If injury is because an artery got plugged then the dead tissue follows the wanderings of the artery. That can cross a variety
of functional types as well as anatomic spatial representations.
Anoxia will damage whatever tissue has a high metabolic rate - needs oxygen most. Most cellular.
High carbon dioxide will damage whatever is most sensitive to that. The term "asphyxia" is used in technical conversation to
mean low O2 AND high CO2. So a placenta not delivering O2 may well remove the CO2. An umbilical kink can make low O2 and high CO2.
An abnormal hemoglobin can do a range of things including pH damage - yet another way. Poisons, viruses, bacteria, trauma,
vitamin glitch, it goes on & on & on.
Damage can be and usually is both sensory and motor. Sensory also includes all that stuff that sorts out input so as to map the environment.
Then there are the kinds of motor consequences. A common one, the MOST common one, spasticity is actually a spinal
circuit phenomenon caused by missing modulation from the brain. Circuits that are capable of very fast reaction normally work under restraint from above. As what is happening oddly is
spinal and well away from anything directly conscious, things that happen oddly feel like they are INFLICTED. Spasticity is happening TO the person.
As you go higher in the central nervous system with abnormal motor output, it takes on a veneer of consciousness and high
enough a sense of will. So dystonic movement coming from a sparking zzzt zzzzt zzzzt zzzt in the caudate nucleus or some diencephalic ganglion becomes a trait. That's how I am.
Dystonic postures tend to be owned by the patient and even sought. A dystonic leg posture carefully thwarted by a large surgical procedure may well have the patient in the recovery
room asking the nurse to please "put my legs over there?" (back to where they were). Sideways in bed uses blankets to sweep the odd postures back. Dystonic postures seen in a
mirror are recognized as odd but feel straight.
We distinguish rigid stiffness from dystonic stiffness, from choreiform and athetoid high tone, from spastic and definitely
from secondary direct tissue contracture. They act differently. They have different sources. They require different interventions and respond differently to drugs.
If you want to really understand this field of medicine then embrace the term "rehabilitation engineering". It isn't
orthopedics. It isn't neurology. It isn't physiatry. It seldom pays much attention to 'THE diagnosis' as that seldom even slightly embraces the problems for which relief is being sought.
It is about inventory. WHAT IS STILL INTACT? What can be used to substitute for what is missing. A big problem is hope.
?
The problem with HOPE:
Oh, come on! You KNOW. Hope is a disguise for denial. It is
passive. Waiting for angels, for that new drug, or embryonic fuzzy logic cell that resets the clock to birth. Do SPMLs make the diagnosis go away? Stem cells? Lots of oxygen?
We do not deal in hope. We deal in observation and inventory. We need and carefully apply neuroanatomy to making our assessments.
Rehabilitative engineering. Step one is clean your eyeglasses.
Step two is roll up your sleeves. ... reality is on the run. It is up to us to catch it.
|