|
OK folks, hush up and be seated. We have a super duper visiting professor today.
Dr. David Yngve (pronounced DAY-vid) brings very special
skills and experiences and a great topic - plus he's a sailor, what's not to like?
What? Oh. (say Ing-vee).
He has had a long experience with analysis of human motion, walking pathology, and well planned interventions. He is one of those
analytic thinkers who swats the irregularities of entrenched theory. He could talk on so many topics (maybe we can squeeze more out of him) but he thought we were a bit thin on this subject ... yup.
|
|
 |
Walking for someone who has cerebral palsy can be full of challenges. There can be problems with spasticity
making balance difficult and problems with fast reactions leading to tripping and falling. But also there can be
problems in the hip, knee and ankle areas. At the hips, there can be excessive groin tightness and spasticity in the
adductor muscles causing the knees to rub together in walking, which in its marked form is scissoring. There can be
excessive calf tightness and spasticity causing walking on the balls of the feet with the heels up. And there can be problems with the knees. Here we will deal with the knees.
Crouching knees
Often those with cerebral palsy will walk with the knees bent, in the crouched position. Why does this happen?
One appealing idea is that those with normal legs will crouch when they are trying to keep their balance. Look at
someone riding a surfboard, unless they are highly skilled, they will be down in a significant crouch to try to go
longer on the wave before losing their balance and falling. But is crouch just about getting low for better balance?
Another tack is to look at the muscles that work the knee. Are the muscles that bend (flex) the knee winning out over the muscles that straighten (extend) the knee leading to a flexed knee position?
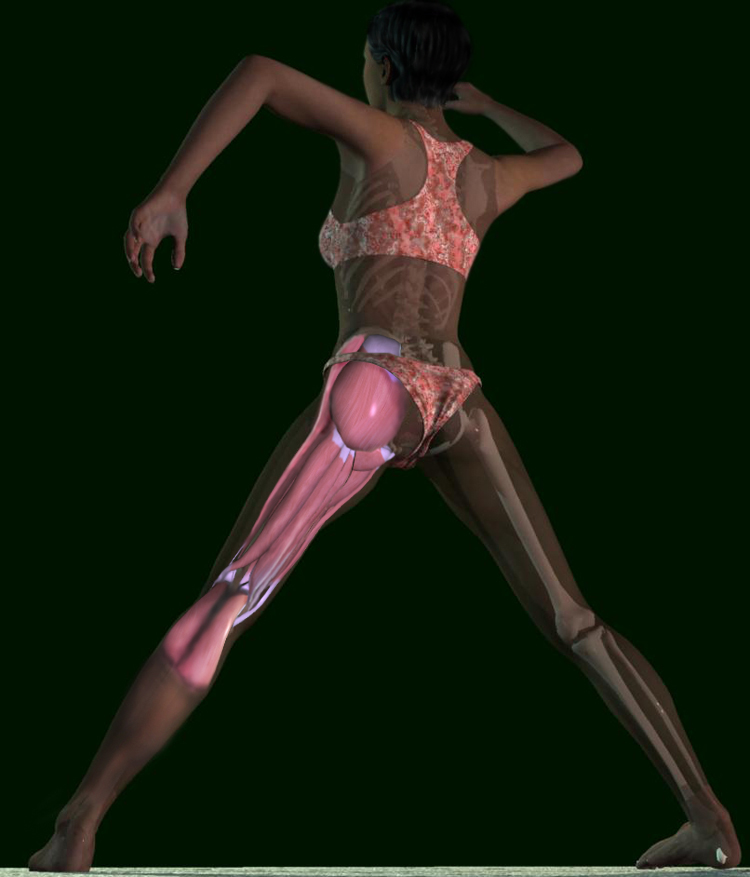
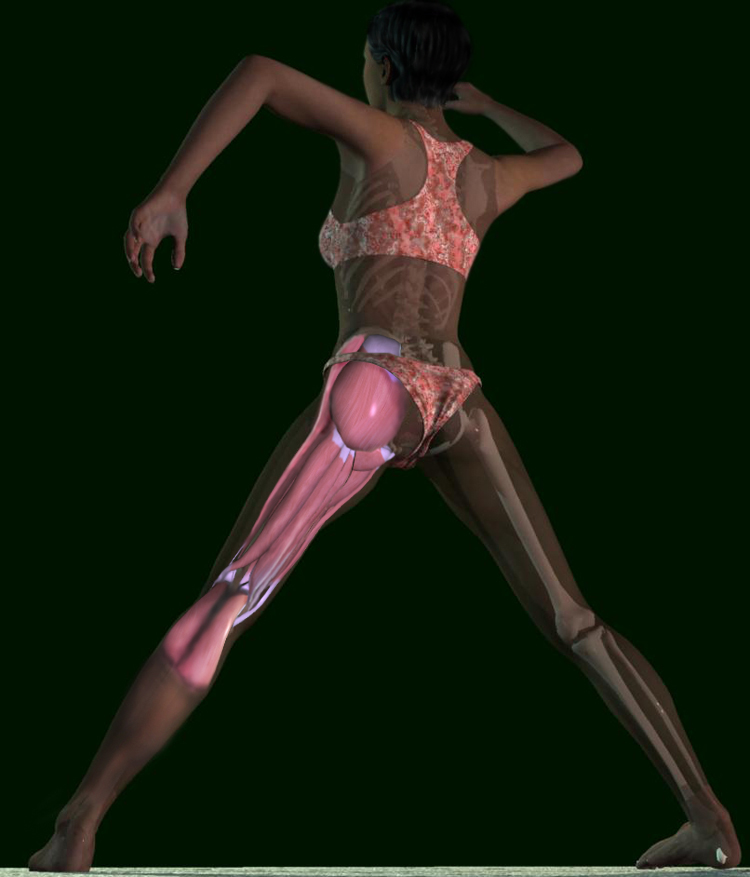
 Knee muscles (hover pointer over muscles to see names) Knee muscles (hover pointer over muscles to see names)
Let's take an inventory of the knee muscles. The muscles that extend the knee are located on the front of the thigh.
They are called the quadriceps and as indicated by "quad" there are four of them. The muscles that flex the knee are called the hamstrings, and there are seven of them. This
looks like an unbalanced situation already, four muscles to extend the knee and seven to flex it. Would the hamstrings win out and cause a flexed knee position? However, in terms
of size, the hamstrings are more slender. When you look at the cross sectional appearance, the comparative bulk of the quadriceps and the hamstrings is about the same with the
bulk of the quadriceps actually appearing a little greater than the hamstrings. Why then is it so common for those with cerebral palsy to stand and walk with the knees in the crouched position?
One joint muscles
There are two types of muscles, one joint muscles and two joint muscles. One joint muscles are the basic type that
extend the knee. The way they work is straightforward. The muscles pull on the knee cap (patella) toward the hip. The patella is connected to the upper part of the lower leg bone
(tibia) by a very stout rope like structure about the dimensions and strength of three strands of ski tow rope laid side by side (the patellar tendon). The muscles pull the
patella, the patella pulls the patellar tendon and the patellar tendon pulls the tibia, causing the tibia to move such that the
knee extends. The muscles attach to the patella on the lower end, where do they attach on the upper end? They
attach onto the thigh bone (femur). There are three of these muscles and they are called the vasti. But what about the fourth muscle of the quadriceps group? This one is a two joint muscle.
Two joint muscles
The fourth muscle of the quadriceps is the odd one, it is a two joint muscle. At the lower end it attaches to the
patella like the vasti do, but at the upper end it does something completely different, it follows along the femur,
going higher and higher toward the hip, but does not attach to the femur. It finally finds an attachment point above
the top of the femur on the pelvis. It is a two joint muscle because it crosses both the hip and the knee joints. So
the quadriceps group contains three one joint muscles and one two joint muscle. What is the makeup of the hamstring group?
 |
 |
Looking at the hamstring muscles, where to they attach? On the lower end, they all attach to the back of the leg,
just below the knee, five on the inside and two on the outside. On the upper end, six of the seven cross the hip joint
, attaching onto the pelvis, and are two joint muscles. Only one attaches to the femur and is a one joint muscle. So
now let's review the score with the one and two joint muscles. The quadriceps has three one joint muscles and one
two joint muscle. The hamstrings have a single one joint muscle and six two joint muscles. Could it be that the two joint muscles of the hamstrings are causing crouch?
Muscle spasticity
Two joint muscles tend to be more affected by spasticity than one joint muscles. A one joint muscle has just one
task: move one joint. A two joint muscle has a much more complex function: move two joints. Consider the
possibilities. A person could hold their upper joint locked in position and move their lower joint. They could hold
their lower joint locked in position and move their upper joint. They could move their upper joint slowly and their
lower joint quickly. The possibilities are endless. It would require nimble brain control to handle all the
combinations and to do the right thing. In cerebral palsy the computer that controls the legs, that part of the brain,
may have good basic function, but may not be perfect for complex problems like working two joint muscles with
perfect coordination. The result can be spasticity in the two joint muscles. It is as if they are contracted into a state
of indecision. How might this relate to crouch? The quadriceps have one potentially spastic two joint muscle and
the hamstrings have six. It seems reasonable to conclude that hamstring spasticity could overpower quadriceps spasticity and could lead to crouching at the knee.
 |
Hamstring surgery for crouch
Hamstring surgery is in general very effective in diminishing the crouch posture in those with cerebral palsy. With
percs (SPML) surgery the two joint hamstring muscles can be easily lengthened. Of the six hamstrings that are two
joint muscles, the number of muscles that are lengthened depends on the particulars of the case, but can range from
two to four. A good result occurs when the most affected muscles are lengthened, fortunately it is not necessary to
lengthen all of them, since this could lead to weakness. By only lengthening some of the muscles, several remain
intact, which allows faster recovery after the surgery. The lengthened muscles usually have less spasticity. They
are less tight after lengthening. A tight hamstring gets a good strong yank as the knee extends during walking in
preparation for taking the next step. This yank tends to trigger spasticity. After lengthening, the hamstrings are not
so tight and less spasticity is triggered. The result of greater hamstring length and less spasticity is a more erect
posture at the knee. Because there is less spasticity, the knee can make faster reactions, so the legs can move back
and forth more rapidly while walking. Also, since the knees can extend better, they can reach farther forward while
taking the next step, and bigger steps can result, also leading to a faster walking speed. Faster reactions are also useful for catching your balance when you trip, so falling can be less.
Quadriceps spasticity
With six of the seven hamstring muscles potentially spastic compared to only one of the four quadriceps muscles,
hamstring spasticity can predominate and contribute to crouching at the knee. The potential for spasticity in the one
quadriceps muscle that is a two joint muscle doesn't usually display itself as a problem. However, everyone with
cerebral palsy is different and occasionally there is someone who is special in this way. About 5 percent of the time
the two joint quadriceps muscle (rectus femoris) does cause a noticeable problem. Normally in walking the
quadriceps tenses when the foot is on the floor and the knee is supporting the weight of the body. The muscles
tense as if the knee is pushing down on the floor. The muscles have to support the weight of the body and have to
be quite strong, and make quite a contraction to keep the knee from buckling. Then when that foot is picked up off
the floor to swing forward for the next step the quadriceps muscles should be relaxed, so that the knee can bend,
lifting the foot up so that it does not scuff against the floor. Yet, some with cerebral palsy do scuff their feet on the
floor and sometimes trip and fall. And not surprisingly, most often it is the two joint muscle, the rectus femoris that
causes the problem by being spastic and overactive. Its activity prevents the knee from flexing. And at times this is
enough of a problem to think about a surgical treatment, and the best treatment turns out to be something different from a perc.
Rectus tendon
Surgery for the overactive rectus femoris is relatively new, and it is interesting to see how the current state of the art
has developed. The types of surgeries that are done can change through time due to constant improvement, similar
to the way in which today's cars have become superior to the cars of the 1950s. The earliest surgery for the
problematic rectus femoris was the rectus femoris release. The rectus femoris has a muscle in the thigh which blends into a tendon at the lower end about the size of two pieces of clothesline held side by side, which then
attaches to the patella. The thought was: the rectus femoris is causing problems in the swing phase of gait, it is
not needed in the stance phase of gait because the three vasti can handle that part, so let's just cut it loose at the
tendon end and take it out of the picture. This is the rectus femoris release operation. What was the result? Rectus
spasticity and contracture were reduced at first, but then after about 3 months the problem came back. What
happened? After cutting the tendon, the ends separated about a half of an inch and formed a gap. But the body
was able to bridge the gap and reconnect the ends. Being resourceful surgeons they came up with a clever modification, they cut the tendon as before but then removed a two inch section of the tendon to keep it from
reattaching (rectus tendon excision). The result? Good at first, but after 6 months the rectus spasticity and
contracture had returned. The body had again filled in the gap. Dr. Nuzzo calls this salamandering. If you cut the
tail off a salamander it grows a new tail. If you cut a section out of a rectus tendon, it grows a new tendon. Our
bodies are remarkable and wonderful. But the surgeons still had a problem with a tight and spastic rectus femoris. The next solution arose in the 1980s, the rectus transfer.
Rectus transfer
The thought was to move the attachment of the rectus as a tendon transfer. The idea was to take the rectus which
normally functions to extend the knee, and attach its lower end to the back of the knee where it would work to flex
the knee. A good plan, since with these kids, the problem was excessive knee extension. When this operation was
done and compared with the rectus tendon excision cases they were pleased, the problem with excessive knee
extension in swing was minimized and the result was maintained for several years after the surgery. Further studies
were then done to actually map out the new path of the transferred tendon. Was it in a good position to flex the
knee? Surprisingly, the path of the tendon was found to be close to the axis of rotation of the knee joint. For the
tendon to be positioned to flex the knee it would need to be placed further toward the back. Yet the results still
were satisfactory in terms of allowing the knee to flex in swing. The function of the rectus transfer must have been
to take the rectus out of commission only, the thought of it doing the second function of flexing the knee was not
realized, and not needed. Most recently a report looked at long term results following rectus transfer surgery.
When gait was analyzed a year or two after surgery and then again at an average of nine years after surgery they found that there were good benefits early but that the benefits of the improved knee flexion in swing were lost at
the later followup date. Was the transferred tendon also healing back as it did after the rectus excision surgery, just
taking 10 times longer? Should even more distance be created between the tendon and the patella to prevent it from growing back?
High rectus transfer
High rectus transfer is a new procedure that places twice as much distance between the tendon and the patella in
an effort to prevent it from reattaching, even after nine years. This procedure can be easily done along with percs
as an outpatient surgery. It is similar to rectus transfer surgery, but the end of the tendon is set at about the mid
thigh level instead of just above the knee. In my experience, children who have had this surgery have also been
more comfortable after surgery than those who had the conventional rectus transfer surgery, probably because knee
irritation is minimized. The surgery becomes a thigh surgery instead of a knee surgery and thigh surgery is much better tolerated than knee surgery.
|
 David A. Yngve, M.D.
David A. Yngve, M.D.
 Knee muscles
Knee muscles