 |
 |
 |
 |
Braces
Orthoses
Naming:
What's the difference between a brace and an
orthosis? Just the spelling and pronunciation. When "brace" became a negative feeling word, the linguists shot out orthosis. Now we have some kids asking not to call them orthotics, "They're braces!", the cycle of life and
language.
Orthosis = 1, Orthoses = more than 1, Orthotic is an adjective (like blue) but which often has its noun dropped (orthotic appliance) - hmmm -out of the blue.
We know that a brace braces. An orthosis? It braces too, the linguists were lazy. An orthosis is applied to a body part. A prosthesis replaces a body part. Braces used to be named to sound similar to the closest prosthesis type. A below knee prosthesis replaces a missing ankle and foot. A below knee orthosis braces the ankle and foot. What do you call an orthosis that does that? It is an AFO. AFO? Meaning?
Nowadays, because there was a meeting where this was decided, you just string the first letters of the parts to be held appended by an "O" for orthosis. HKAFO = hip-knee-ankle-foot-orthosis. TLSO = thoraco-lumbar-sacral-orthosis, and so on.
Concepts:
Braces serve more than one purpose.
They:
1) mold shape with growth
2) promote a position needed to perform certain tasks
(maybe even making other lesser tasks less easy)
3) keep certain muscles and tendons stretched out (act as stretching time).
The most common error in considering braces is to not consider all three categories and rate them as to relative need. A three year who can walk even when she takes her brace off, might be set free of braces only to have the condition which required the braces, return. Under each category consider attain & maintain. The latter is especially important in the wee ones.
Another oversight is that sustained pressure on skin that is over 7 pounds per square inch will cause pain and break skin. Well made braces will cause sores if asked to hold too much deformation force with too little surface area.
By Location:
Most really effective positioning hand braces interfere with
fine activities. Braces that do not so interfere, typically are less successful at postural maintenance. Typically, when both are important, we use two braces and trade between them according to activity. The more severe braces
generally are worn at night an between activity periods. This is especially true of hand-wrist braces wherein we are most interested in fine activity.
Larger supportive braces as worn on the foot have infrequent need to be swapped as fine control is a lesser demand in most cases. But there are some.
TLSO (back braces) see the discussion in the scoliosis section.
HKAFO - so called "full control braces" - they hold the hips (and so must be above the hips). They also hold the knees, ankles, and feet leading to the alternate name "no control" brace depending upon the perspective - patient's or brace's. A brace that braces so much certainly controls much. However, brace control, fine for static postures, is no substitute for muscle control as needed to function. They are most suited to transitional conditions where the disorder is at its worst or in cases where no functional control exists, and therefore is not impaired by "full control" bracing.
To stand, in such braces, the hips must both fully extend. Knee contractures will place huge collapsing counter-force needs on the brace which cannot be tolerated by skin. So knees must be near or slightly past full extension.
The ankle component is always
judged with the shoe included. The bottom of the shoe (the floor) and the shin ought NOT be a square angle - so called "neutral". Neutral position is a throw back to worship of the false god Euclid. Euclid did not design mankind. His concepts are not embodied in the biologic plan. In stance, braced and unbraced, the shin is tilted forward about 7 to 14 degrees off vertical, not 90 degrees off horizontal.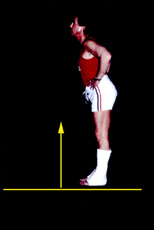 The ankle is not at the center of the foot. To get body center over the
center of our base, we must tilt the upright support (legs) forward, otherwise there is a need to flex at the hips sharply to compensate (jack-knife posture). Most cases of kids standing flexed at the hips are from
this oversight. Most. Not all.
The ankle is not at the center of the foot. To get body center over the
center of our base, we must tilt the upright support (legs) forward, otherwise there is a need to flex at the hips sharply to compensate (jack-knife posture). Most cases of kids standing flexed at the hips are from
this oversight. Most. Not all.
This normal volunteer has casts on his ankles which hold his feet downward so that his legs are directly backward. He must flex at the
hips or stand on his toes to balance. Square floor to leg does likewise, but just to a lesser degree. The shoe must be considered as the heel can offset the braced ankle-foot squareness, depending on heel height.
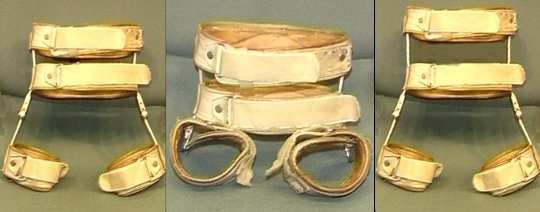
 TKAFO - or just KAFO - Thigh knee ankle foot orthosis. Sometimes these
are used just to provide protection of knee ligaments, especially in kids with spina bifida, when walking has the knee getting slammed with each step. It
isn't so much the position the brace as a positioner but as a hit taker. Other times, as we see here, it protects a brittle bone. Those that are protection braces are more apt to engulf the part. The old lacers are very well
tolerated by kids with trouble skin. Joints are either free to move or constrained and may even be locked or able to lock and unlock as need dictates.
TKAFO - or just KAFO - Thigh knee ankle foot orthosis. Sometimes these
are used just to provide protection of knee ligaments, especially in kids with spina bifida, when walking has the knee getting slammed with each step. It
isn't so much the position the brace as a positioner but as a hit taker. Other times, as we see here, it protects a brittle bone. Those that are protection braces are more apt to engulf the part. The old lacers are very well
tolerated by kids with trouble skin. Joints are either free to move or constrained and may even be locked or able to lock and unlock as need dictates.
 AFO - The Ankle foot orthosis is one of the most varied in form and in applied mysticism. The "below knee brace" has been justifiably called the baloney brace.
Here are two versions: left & middle = solid ankle, right = hinged (with a rear strap that can set a forward limit or motion and a rear stop to prevent "Euclid's Backlash". The toe plates are
flexible back to the ball of the foot. The braces totally contact the anatomy.
AFO - The Ankle foot orthosis is one of the most varied in form and in applied mysticism. The "below knee brace" has been justifiably called the baloney brace.
Here are two versions: left & middle = solid ankle, right = hinged (with a rear strap that can set a forward limit or motion and a rear stop to prevent "Euclid's Backlash". The toe plates are
flexible back to the ball of the foot. The braces totally contact the anatomy. Spiral AFOs are buggers to make and therefore hard to find. They allow a limited arc of motion in all directions and can favor one direction over another as an assist.
What they really do well is transmit ground pressures to higher skin and provide proprioceptive cues (touch and pressure) that may be absent in the foot. By allowing small arc with low resist and moderate arc with more
resist, the damping of motion is very physiologic. It is also the basis of the proprioceptive quality (which would be dissipated if there were larger surfaces. The is
no toe plate at all so as to allow optimum toe sensibility. The numbers of persons who "need" this kind is small, generally when dystonia and athetoid properties require some help. The latter
patients often do terrible in good braces as they can't tolerate "excellent" immobilization.
Spiral AFOs are buggers to make and therefore hard to find. They allow a limited arc of motion in all directions and can favor one direction over another as an assist.
What they really do well is transmit ground pressures to higher skin and provide proprioceptive cues (touch and pressure) that may be absent in the foot. By allowing small arc with low resist and moderate arc with more
resist, the damping of motion is very physiologic. It is also the basis of the proprioceptive quality (which would be dissipated if there were larger surfaces. The is
no toe plate at all so as to allow optimum toe sensibility. The numbers of persons who "need" this kind is small, generally when dystonia and athetoid properties require some help. The latter
patients often do terrible in good braces as they can't tolerate "excellent" immobilization.
A study funded by the U.S.Navy (see cv) took the most practical approach possible (after
extensive gait analysis still left all the could-be would-be should-be coulda-been theories untouched). Selected patients representing varied needs and diagnoses were given shopping
bags full of AFOs of every conceivable form. The instructions were easy. Try them all. The kids were rated as to function and appearance by themselves, parents, and by our
measurements of function. We were expecting a massively complex result. That did not occur.
Only two things were important. Ability to hold a shape, that is shape a foot and the geometry
of three points in space (Knee, heel contact point and forward roll over point).
Holding shape: Pretty obvious, the better the fit and the contact and the less flimsy the better
the shaping ability.
Walking: Well, you have already read the facts above. The foot at midstance ought to have the
knee ahead of the ankle (shin tilts forward by about 10 to 14 degrees). The forward rolling point is at the metatarsal heads and NOT the toes. A stiff toe plate or a shoe reinforced with a
lift creating a stiff toe area ruins walking. The brace wearer will try to get the toe out of the way in that case by turning which ever direction is easiest for them (inward or outward). If unable to
do that we see a body lurch (hip jack-knife on the fly) as the leg abruptly slows but the body continues.
A solid ankle orthosis meeting the three point geometry does better than hinges in some kids. Why? Range of motion without control is falling, or a crap shooting at best. The randomness of uncertain foot placement deprives a walker of the speed allowed by expectation (see walking).
Now walking is one thing. There are other things. Playing on the floor, squatting, climbing a cyclone fence with a dog after one's backside. You must consider which activities are most near and dear. If there is SOME control in the muscles, allow that DEGREE of freedom, but not more. Some kids will actually show more varied and complex skills with less controlling braces (spirals, low SMOs etc), fine but watch foot SHAPE. Occasionally we give up the cyclone fence leaping to sustain foot shape through the early growing years. The taller braces prevent muscle and tendon contractures better but may be overkill for play activities. Two brace kinds are ideal but insurers don't want to hear this. Life is compromise.
 What is the name for a hinged AFO that allows free plantar
flexion? We call that a Landfill orthosis, that's where they belong.
What is the name for a hinged AFO that allows free plantar
flexion? We call that a Landfill orthosis, that's where they belong.
Here is one. It has a stiff toe plate as well. mmmm
Spica casts are often used to hold legs after surgery. They are nasty, but often all there is. But some surgery does not need that much hold and some
 |
 distance apart). Here is a trap.
distance apart). Here is a trap.The eye sees the space between the legs whereas what is important is the orientation of the THIGH to the BODY. A wedge between the legs may well separate the legs, but it may also allow one leg to cross midline (adduct). A simple hip ring might wind up at an angle across the pelvis. Kids who "wind sweep" (both legs go rightward or both go leftward) will adduct one leg for sure in any "A-frame" or wedge brace. You need a body reference. The above braces serve this need. The upper rings just define the torso. Each thigh is looped by a cuff to either abduct the legs (as with the fellow seen here) or closer together to merely prevent legs crossing mid line until the condition or surgery heals. The hinges allow motion including sitting and standing.

Metallurgy is also a consideration. A brace to correct Blount's disease is an example. In that condition braces can be used effectively in early cases, but they are not easy braces to make as the thing to be shaped is
bone. Bone does not just go from here to there without a crack. We are nudging the growth zones.
This must be a nudge below the 7 pounds per square inch skin
tolerance but yet be multi-directional. These kids have both leg angulation and twist.
The brace is applied to fit the deformity. Then, the brace is reshaped
(metal is twisted and bent) in the direction of correction in small frequent intervals. The metal must allow small incremental twists and
angulation alterations without being too weak such that it breaks. Such braces only apply twist forces when they are flexed and apply angular forces when they are straightened, giving the
skin the intervals of pressure relief that is required. Without a brace maker who really understands these requirements it just can't be done.
An important fact... a really really super duper important fact:
In the presence of sensory defects, most of this reasoning falls apart. Sensory defects can and do look alot like motor defects. You need to be attuned to the subtle clues. Attuned you succeed. Not attuned you go down in flames. So don't avoid the SENSORY section.