 |
|
|
|
|
||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||
|
OK, place your hands on your hips. That spot is the top of the pelvis (near the waist). Shapely hips? Closer, but that is a region, not a joint. Guess how many bones make up the 'hip joint'? Did you guess four? There are two main parts, the femur with the ball top and the pelvis with the socket. The socket is made of three joined pelvic bones - the ilium, the ishium and the pubis.
|
|
But if you look closely at that pelvis, you can see that it is a composite bone - not too unlike the skull - wherein several bones join together to create a single functional structure. The three sub bones of the pelvis are called innominate bones (in-ohm-min-it) because orthopedists mastered saying "The Leith police dismitheth us." and thus needed something harder to say.
Those innominate bones in your tush, the ones which you sit on, are the ishium bones (ISH-she-YUM). The last innominate is the pubis which completes the birth canal ring of sacrum, iliac, pubis-pubis, iliac, sacrum. The great coming together of the three innominate bones is at dead center in the hip socket (acetabulum, say ahh-suh-tab-you-lum). The femoral head nestles into the socket formed by these three bones and embraced by the sleeve of "capsule" tissue that encircles and contains the "hip joint."
Notice that the contact area of the cup is not the entire socket, but rather a horse shoe or inverted U zone around the socket's edge. An open notch at the bottom is spanned by a ligament. Fat gains access from this lower notch. Another ligament spans from lower notch to the femoral head. To the left, point downward, is the sacrum. Thescooped out area in front of the sacrum but behind the hip is the sciatic notch. A big nerve we all know and love leaves the pelvis and enters the leg at that notch. Guess kit's name. No, not the notch nerve. Well below that are the ishia on which we sit (some of us more than others). This location is a source of skin breakdown when sensation is lacking and the tissue does not warn us that it is time to fidget. Oh, by the way, figeting is good. It prevents pressure sores.
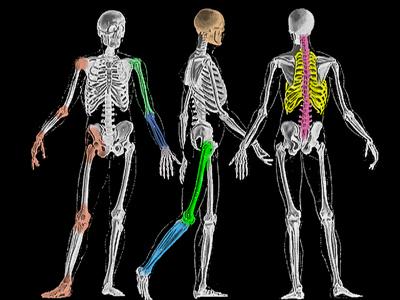
The blue areas are cartilage in babies. At birth, the small boney center of the femoral head is not yet present, nor is that of the greater trochanter. A line drawn down the center of the neck of the femur as seen on x-ray is not at all in the center of the femoral neck, just the center of the ossified (bone material) femoral neck. The Teres Ligament attaches to the ball of the femur and at its lower end to the lower notch area of the acetabulum (socket). To dislocate the femoral head, this must be divided (very unlikely) or stretched out - the usual. As the ligamentum Teres stretches, it reconstitutes itself in girth so that it may be many times its original size and volume in cases of developmental hip dislocation. To put the hip back in the socket may well require removing this structure. The green line shows about where the capsule, a sleeve of tough ligament tisue, attaches near the base of the femoral neck. Backward motion of the leg may well be stopped by the limit of this tissue as it tenses from tugging at the top of the socket where the fibers of the capsule converge. At the stop point, that capsule - at its max - becomes a force fulcrum. Further extension force pivots on this line pressing the femoral neck forward from below and the femoral head (trapped in the socket) is pressed backward and a bit relatively to the neck. That is resolution of anteversion.
In small daily nudges this may well be how the entire upper cartilage gets translated backward. You see, the femoral neck points more forward in babies and less so by early teens. The island of cartilage between the femoral head and greater trochanter disappears first. That leaves the head connected to the neck by a transverse plate of cartilage - the physis - or growth plate. That same backward force of the femur against the limiting capsule will stop further leg extension or - if the growth plate is thick and weak enough with enough leverage - drive the head backward and down on the neck. That's a slipped epiphysis. If it is bit by bit, the cartilage deforms and heals, deforms and heals with gradual slippage without anything coming apart. Given enough force or weakness, it just plain breaks. That's an acute slip. When the femur bone gets divided for correction of congenital or developmental dislocation, that is usually done just below the lesser trochanter.
H = a horizontal line drawn between the two triradiate cartilage centers of the hips defines a
horizontal planne and an approximation to flexion axis of the hips. Hilgenreiner's Line S = an oval that traces the lower pubis contour, ought to smoothly continue on to trace the lower edge of the neck of the femur. Shenton's Line. In this case, Shenton's line is off and discloses that
the femur is migrating upward as these shallow hip sockets do not satisfactorily contain the ball in the sockets.
At the turn of the century (uh.. the last turn, that is - 1900's) dislocated baby hips would have been likely to be left that way. A side to side waddle gait with substantial sway back would have been the result. The femurs would sit high adjacent the iliac wings or even in the sciatic notch area. The hips sockets would wizen away and the femoral heads lose any trace of roundedness. The pelvis is then suspended on ligaments like a swing from a swing frame.
Then surgeons got frisky and began to try putting the hips back where they belonged. Anesthesia made that possible. Possible - but not easy. There was much to be learned.
True enough that muscles had to be relaxed, but longstanding dislocation produced physical shortening of muscle and ligaments that went beyond active tension.The techniques of placing the dislocated femoral head into the socket in DDH (developmental hip dysplasia) are fairly old. The methods reflect the learned pitfalls.
Traction, protracted pulling on the leg, did stretch the tissues to allow easier manipulation of the hip into the socket with less pressure required to hold it. Even so, forces were still high and those forces caused enough bad hips (stiff and painful to the point that many pediatricians were against surgeons relocating baby hips as the dislocated state seemed preferable). Besides, then, a lot of women waddled (girl hip dislocations outnumbered boys by about 9:1, see the general hips section for why).
The biggies were the hip adductors and the much deeper iliopsoas (a dual muscle made up of the iliacus muscle whose origin is the iliac bone and the psoas muscle whose origin is the pso..uh.. no - its origin is the spine. That worked! The 80% complication rate - it was that high - fell into tolerable numbers. But that improved further when additional tissues were understood and removal of blocking tissues was added for those that did not go back (reduce) as was hoped. The ability to see inside the joint by injecting "contrast" into the joint before taking x-rays ( radiologists correct us when we call it dye). But there were still pesky ones that did not stay put and that twisty leg posture of varus and derotation was hard to just toss - hip damaging as it was. An operation that essentially positions the hip this way, but divides the shaft of the femur from the hip and returns the rest of the femur segment to straight ahead posture (using metal screws and plates to hold the two fragments in the new relationship) was developed.
The pressure is less with VRO due to the muscle releases that accompany it and also due to the shortening of the length of the femur bone which occurs in the process. Creating less length for muscles and ligaments to span releives pressure. Indeed, the trick of shortening bone rather than (or in addition to) lengthening muscle and whatever else was so successful that shortening is used straight away for very severe cases even without varus or derotation. Because leg muscles attach to the shaft of the femur, taking out a section high up allows the head and neck piece to drop down. So, in fact, a shortening of the femur bone does not FURTHER shorten the leg (which is already foreshortened) , but keeps the leg where it is as the head and neck are dropped into place. The overlap is cut away to allow the two parts of the femur to be secured to one another by plate and screw fixation.
In a number of conditions, pressing need and persistance maintains the roundness required of flexion-extension. However, the sideways and/or vertical motion may suffer to hip shape deformity. In those cases the hip has become cylindrical or egg shaped rather than spherical. The shape of the femur head may match the socket in one plane but not another. That will reflect in a stiff mechanical look to the walk. Supple side sway of the hips becomes difficult to absent.
|
|
|
||||||||||||||||||||