|
S.L.O.B. aka Summit Shelf
or B3 Hip augmentation
Fig. 1) Hip socket augmentation is done for a variety of reasons. The most common
, in handicapped persons, is to deal with a dislocating hip.
In that setting the hip dislocates because the hip socket is too shallow
and the shallow socket is also too vertical (socket facing outward rather than downward). In standing, the
ball tends to piston vertically in the dish shaped socket and even slide out. Ways to treat this are many and often used in combinations.
Fig. 2) The upper end of the thigh bone might also be insufficiently angled (Too straight
= 'valgus') to point the ball toward the socket center rather than toward the socket outer edge. Cutting the thigh bone to angle the upper femur more sharply into the socket is
done at times. It is the most common late treatment used. The disadvantage is that this femur surgery ( Fig. 3 = Varus osteotomy or VRO etc.) shortens the leg and causes the leg to track oddly when transitioning from sitting posture to standing. It is big surgery with
a large metabolic demand for healing. Healing to standing time is about 12 weeks. A hip metal 'nail' is needed to hold the angle until adequate bone bridges the cut. The metal is
typically removed about one year later. Loss of position of the held piece is not rare,
especially with soft bone or very tight spastic reactions that can overcome the metal hold on the bone. Such slippage has the potential for further revision surgery.
'Innominate
' (or pelvis) osteotomy repositions the hip socket itself by cutting the pelvis around the socket and swinging the socket itself to a new orientation - more horizontal. A
wedge bone graft is used to secure the new configuration by filling in the gap created by moving the socket. Threaded pins hold the graft. Leg length is not changed much, as the
rotational shift occurs nearly through the center axis of the hip itself. It does not deepen the socket. It just tilts it more horizontally. The hip socket goes from being positioned like
an ear muff to more like a cap. With a very shallow socket, the result may be merely that the dislocation occurs in a different direction.
Fig. 5) Some cases of instability from shallow structure can be dealt with by building out
the edge of the hip socket with grafted bone. (acetabuloplasty). Bone from elsewhere on
the pelvis can be used. That bleeds and increases blood loss. There are many techniques for building out a shelf over the shallow socket. Some are very old, indeed. This is not a
new idea. It is, however, sizable surgery which gets even bigger in that surgeons had to get their bone materials from another or adjacent site - more wound, more bleeding, more
post operative metabolic demand in healing the main surgical site as well as the donor area.
 Alternately bone bank sources are used. Simply, banked bone is similar to transfusion -
risk wise. Alternately bone bank sources are used. Simply, banked bone is similar to transfusion -
risk wise.
We developed a much safer simpler method employing a two phase industrial mixture. It has
proved very effective, cuts morbidity significantly and lessens post operative demands.
One component of the mix is structural. It establishes the area which is to become bone. It is
invisible on x-ray. This component acts as a scaffold, a filler, on and in which the body places its own NEW bone.
A second component is a bone stimulation agent which drives the body to form bone on the
scaffold which is absorbed as replaced by real new bone.
New bone forms faster this way. It is easier to track by x-ray than when native bone is
used. Bone seen on x-ray in the graft area is new bone as the materials used do not show. We prefer this method developed by us soon after the separate components were made available.
We have named this procedure by the conventional descriptive location method (superio
-lateral outcropping bone graft which has the unfortunate acronym SLOB). The more
tolerable name has become the "Summit Shelf" (SS) although the procedure does not actually make what is typically called a shelf, so that's a bit confusing. B3 (big blob of
bone is actually a better description than shelf yet does not satisfy why the SLOB term was used in the first place.
OK. WHY?
Some radiologists reading one month post operative x-rays and not knowing what was
done were diagnosing sarcoma!! GAD!! The SLOB term was usedon the x-ray request forms in the long form to point their attention to the superolateral bone graft they were
seeing on AP x-ray and it's supposed to be there. There is more bone than that but that part is what had them confused.
The SS or B3 does not immediately bring new joint surface to the built up area but
merely enhances stability of the hip ball in the existing articulation region. It impedes intermittent lateral displacements which further erode the socket edge. The new bone is
situated outside the hip "capsule", a sleeve of thick flexible tissue. The bone outcropping holds the growing (in younger kids) hip socket soft cartilage edge tilted downward.
That growing edge of soft cartilage material is what gets bent up on impact. When it stays
up from repeated assault, the socket grows taller (up) but not deeper (down and out from the top). That is wh y the socket is both shallow AND vertical in many cases. y the socket is both shallow AND vertical in many cases.
If there is still enough growth left, then the redirection of the soft growing edge allows a
more normal native socket to grow (deeper).
In addition new growth has nowhere to go but under the overhanging bone thus making real
hip formation more horizontal and deeper.
That's another reason we prefer this in the younger kids. The robust (huge?) bone
overhang gradually lessens over a long period, but keeps a good residual to do its job. An intrailiac periacetabular turn down (another new thing to name?) really deepens the
socket and gets the growing edge repositioned under the bone grafted form. New growth happens under this constraining blob. Unlike the long list of innominate osteotomies
named this does not cut THROUGH the pelvis but stays WITHIN it. It does not reorient the pelvis it truly deepens the socket and redirect the edges relative to the pelvis.
The SLOB (or B3) is well suited to cases of early hip 'migration, in conditions of lesser
demand - limited function, household ambulators etc.. Alone, it seldom requires blood transfusion even when both hips are treated. Early migration of the ball of the hip in
dystonia (CP) is our dominant reason for this surgery. A bit fargone for the PREVENTION by SPML, but not so far as to take a hatchet to the pelvis or both femurs
. Still a prevention. Think this way: We see that we are losing the hip structure. It is still OK but won't stay that way as we see things going...=> SLOB.
If a body cast is used (we seldom need it unless other surgeries call for one - really really
rare), it is removed in about 4 to 6 weeks. Rather than a cast, we prefer a brace, which allows the hip to move (can sit and stand), but which only prevents adduction (leg crossing mid line).
Treat the cause. Soft tissue (muscle, ligaments, capsules, tendons) which caused the
problem is treated at the same time. These tissues vary. Lengthening the 'ileopsoas' muscle is occasionally needed (inside the pelvis). This intra-abdominal surgery can elicit a
normal trauma-survival intestinal shutdown reflex called "ileus". Ileus lasts from minutes
to several days. It requires feeding by intravenous route until that protective reflex subsides. The hip surgery alone can bring on that ileus reflex especially when the nervous
system has problems and identifies sources of information badly (can't tell pelvis from intestines - on very close reflex circuits). We have originated a new treatment for this
which uses local anesthesia inside the depths of the surgery even though the anesthesia is general. It seems that the ileus reflex survives general anesthesia but is lessened by local anesthesia (go figure).
Additional muscle surgeries, such as lengthenings are done to deal with the paralytic
causes and to attack functional needs as indicated case by case.
A more generalized concise discussion is found in acetabuloplasty.
Complications
We will update this over time.
All surgery is subject to complications. Let us discuss the known complications of the
SLOB procedure as such discussion appears nowhere else.
The SLOB was developed to avoid, when possible, VRO. Many successful VROs have
unhappy patients. That is, keeping a hip in a socket can be at a large functional loss and/or associated with loss in positional capability. Did it work?
Several children, all early in our series, had bone formation which made the tissues near
the incision feel hard. We have changed the closure methods to reduce that.
In 18 years, three hips have had to be revised for loss of position. That, still exceeds
VRO as effective for the primary goal. Also consider that one sided problems do not require bilateral operations for symmetry as with VRO. However, also note that we still
do VRO and that VRO may be the only stable treatment (in combination with - perhaps - a pelvis or hip socket operation.)
We have had one child drop in function level due to stiffness of the relocated hip..
We had one infection. That infection was actually of the surface tissue and caused by a
rolled up tight diaper that cut in and made a wound ulcer that infected. The close proximity to the bone grafting made us remove that graft, lest it become a pocket for
chronic infection. Large drains were placed and pulled after 2 weeks. The bone had been in place for about two weeks. Interestingly (very), the bone induction was already
underway and went on to create a covering anyway. It wasn't as extensive as our intent but it did do the job. The outcome was good.
We had a run of poor bone formation all at once and in succession. It was clearly related
to a change in procedure. We had adopted a recent standard of adding a certain antibiotic to bone graft. In some bizarre way, that interfered with bone induction in our material.
Even so, there was enough bone formation to still stabilize. Those cases did not dislocate and have maintained position even with the lesser degree of bone shelf.
A recent case was done - under duress - as we actually refused it as maybe going too far.
The family pressed that they didn't want femur surgery and all which that entailed in their very dystonic child with a nearly fully dislocated hip. It was about 98% uncovered or
"perched" as it is called. By the time arrangements were made, it was 5 months later and the hip, on arrival here, was fully dislocated.
SLOB surgery isn't designed to undo complete dislocations. Nevertheless, having
traveled many miles by air and wishing to avoid femur surgery, another very complex operation was performed to avoid femur tampering. In that operation the pelvis was
shortened (to allow the hip ball to be replaced into the nearly absent socket. That socket was substantially reconstructed. In addition, the bone matrix grafting (SLOB) was added.
A spread eagle cast was applied. That worked.
However the SLOB portion which was added as an addition behaved interestingly. At
first bone did form extensively. Later on, follow up x-rays mailed from home showed gradual loss of the SLOB bone calcification along with generalized bone loss from both
femurs as well as from bone in general. There were medication issues which included steroid treatment history and a diet deficient in calcium and vitamin D sources. A call was
placed to the medical doctors to intervene. We have heard that, instead, holistic or herbal methods are being used. That's not good. This case is is being described a "failure" as the
SLOB bone has resorbed about 80% along with the widespread osteopenia. However, the hip has remained located. So this case is a mixed outcome. Best guess is that it will eventually fail.
Another case with very delayed bone formation was one with radiation treatment that
required a spinal fusion to deal with unilateral bone growth arrest (same side as the SLOB). Interestingly, bone did form, just very slowly and the outcome was good.
What we know is that bone induction requires bone forming cells - osteoblasts. They
must be induced to migrate into place and set up shop. Radiated tissue may be very
wanting of such cells. Such cells, once in place, require an intact complicated chemistry which first lays down bone collagen and then calcifies it in a special way. Calcium losing states will not behave well when bone formation is desired. Vitamin D deficiency will
clearly thwart the outcome and even undo it.
We have learned that certain antibiotics, directly placed in tissue where bone is to form -
somehow - defeat the bone cell migration. The class of antibiotics involved has some action on muscle as well as another minor side effect, which may be related.
We have been following a large number of the children so treated. There are trends which
are better seen over this span. One of the primary assertions which led to the SLOB was that the first damage was not to bone but to growing cartilage. Specifically, the edge of
the hip socket is a small overhang that points down and out. Growth is thus down and out
. So a hip socket gets deeper with growth. At the time of the SLOB surgery the socket edge, which has been battered like a boxer's nose and flattened (such that it points up and
the growing hip socket gets taller but not deeper) the surgeon returns the edge to pointing down. The surgeon may turn down the edge or even the entire socket roof and especially the edge so as to redirect future growth down & out.
Future growth. The SLOB acts like a hand outside the cartilage to protect it from getting
battered by the lateral thrusts which you just know are unavoidable in dystonic patients. The SLOB takes the hit and contains the femoral head. But it does not grow. Indeed,
over long spans the very exaggerated low hanging SLOB bone which alarms those who don't know what it is, receeds. During that time the hip muscular issues have been
addressed and native socket growth has produced a deep well formed structure that does not even need the SLOB.
The catch is the growth requirement. Again, the group for whom this was first developed
is the group with the best mechanical appearance on x-ray. That is, SLOB is best for the younger child whose writing is on the wall and that writing is that the hip contour is failing
. Extrapolated, failing => failure. SLOBS have had excellent application in reversing this.
In the more mature hips some form of salvage socket deepening is needed - which we call
an intra-iliac peri-acetabular turn down, while others may use a technique called Dega as the minimum required. In the face of severe femur malrotation which when the knee is
faced forward would direct the ball right out of the socket regardless of depth, then a miracle is needed. That miracle is called VRO - perhaps with femoral shortening.
Another issue is that, whereas VRO produces substantial right - left asymmetry if done on
one side alone, SLOB does not. The end game is that most surgeons using VRO as the only operation will do it to both legs at once even though only a single side is threatening.
We have not done that with the obvious advantage of smaller surgical scope.
However, we have seen a few children who later have gone on to have what was the
good hip now show the changes of socket flattening and migration while the SLOB side looks good. It is a small percentage but a very bothersome observation. Just how good is
good and how minimal a change is best addressed by going to both sides from the outset? Don't know. It is the kitchen sink question. Do you just throw everything including the kitchen sink at everybody?
There are no perfect choices. All we can do is try to dodge the most dreaded possibilities
by opting actions whose problems - in context - seem more palatable, were they to occur. We wish it could be better. We really do.
Update:
Our earliest patients getting the Summit Shelf procedure were
Results were encouraging as this is a very difficult group over the long run. Dystonic
patients can do some very weird and intractable things in response to postural change. Turn their head and arms go into a fencing posture. We saw similar to changing the upper
femur shape. Odd postures in either limb might happen and even persist. Because the SS didn't change any relationships, probably, this was not an issue.
Additionally, the fast healing of the pelvis and of the bone induction material allowed fast
resumption of activity. We were not forced to always do BOTH sides (right AND left) every time in order to get symmetry.
Confession follows: We were right in the middle of a huge surge in AIDS and our region
was second only to San Francisco and I think even surpassed it at one point. Blood banks were maddening in not allowing a single person (mother) to donate more than one unit of
blood. Designated blood was not being allowed. In our area designating blood did allow us to dodge the very high risk areas. We had to use outside private blood banks in order to get designated blood.
By the way, this got to the point where the NUMBER ONE cause of death of "women of
child bearing age" in our state was AIDS (mostly drug related). Druggies were notorious for selling their blood for drug money. To deter professional blood donors the ruling was
only one pint per donor. Hence the problem. That the single donor was a not for money healthy mother was not allowed for. Pooled bank blood or nothing was the official stance
of those who didn't want the extra work of sorting out exceptions.
We became blood aversive. In the many years we have been doing this surgery, only two
units of blood were given. One of those was not by us and maybe could have been held back but it was a fair call for a child having other problems.
Pressure to extend this to older and more advanced cases of paralytic hip subluxation
came from many places. We gradually extended our indications and did do the procedure for those who insisted that VRO was not wanted by them. That left SLOB or nothing.
What did we learn?
Easy cases are easy. Hard cases are hard. This is not being cute. One problem was that
we had only ONE way to treat and that one was and is a big deal with substantial down time and exposure. It did not deal with the hip socket shape but rather relied on
spontaneous socket healing which was a crap shoot.
Furthermore, there was an unspoken reluctance to do something big unless and until
something equally big was at hand. This has led, we think, to waiting too long to intervene or to the routine nearly everybody gets bilateral VRO approach.
For the dystonic kids, the SLOB done in the early phases along with acetabular turn down
(similar to "DEGA") , has done well. The muscle forces are dealt with at that time. Hips have remained in place and even have reverted to being better. VRO could also claim this,
perhaps. But the scope of what is done becomes much greater for the group when throwing the biggest thing at all cases and always both sides.
For the older cases, the single most difficult impediment to doing well is something which
the VRO does address directly. Severe malrotation of the femur bone can twist the femoral head out of the socket when the knees are directed straight ahead. A highly
stable hip socket is one force which causes the femur to grow straight when function directs knees forward. But with wrong function and thus wrong forces through the bones,
growth may get misdirected and the twist of the femur bone can become profound. It can be so severe that when seated the hip ball actually points away from the socket. Given the
huge leverage of that long bone, the twist will win over hip structure.
Secondly. When there has been long-standing hip dysplasia, there has to be significant
growth to allow the reshaping (remodeling) of the femoral head back to roundness. A late surgical "relocation" may relocate a square peg into a round hole without sufficient
growth potential to remedy that. This is also a problem for VRO. Redirecting a femoral head that is out of shape into the socket does not guarantee a decent hip articulation.
We have used the SLOB approach to merely provide a stop point for dislocation
migration so that the leg length difference and abduction loss won't be so severe, but it is not to be thought of as a reconstruction. More of a make do for some very difficult cases
where better options are not to be found.
Let's look at some cases which cover the span of what we see.
 First of all let's consider the things to look for. Even though the lateral
outcropping bone hangs down quite a bit, hip abduction range is reasonably wide (wide enough). This is because we maintain abducted range while the bone is forming. The brace restricts
adduction only. Range of motion (flexion and extension while abducted) during healing is very important. First of all let's consider the things to look for. Even though the lateral
outcropping bone hangs down quite a bit, hip abduction range is reasonably wide (wide enough). This is because we maintain abducted range while the bone is forming. The brace restricts
adduction only. Range of motion (flexion and extension while abducted) during healing is very important.
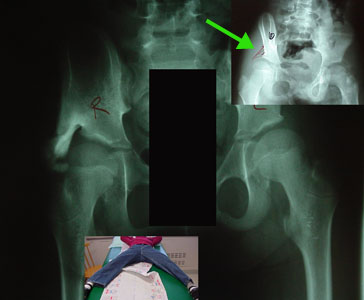
The green arrow
points to a pencil sketch of the "labrum" on the x-ray. Invisible to x-ray, this is the area of the soft growing edge of the hip socket. It should point down & out. If it gets battered to
point up then growth creates a vertical taller saucer-like socket, but not a deeper cup-like hip socket. The ball migrates upward in this vertical saucer and can piston in it, making it
a battering ram as well. That additional battering adds to the speed of worsening.
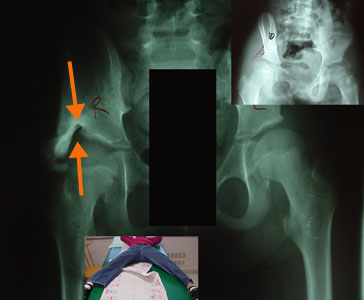 The orange arrows point out a hole in the new bone formation
. This is the location of the tendon of the rectus femoris which is like an eyebrow on the socket. It travels the top edge of the cup. It sits on a rich source of blood as many small feeders
come in right at it's edge which is protected by leaving this tendon in place. It is also a natural cushion. The orange arrows point out a hole in the new bone formation
. This is the location of the tendon of the rectus femoris which is like an eyebrow on the socket. It travels the top edge of the cup. It sits on a rich source of blood as many small feeders
come in right at it's edge which is protected by leaving this tendon in place. It is also a natural cushion.
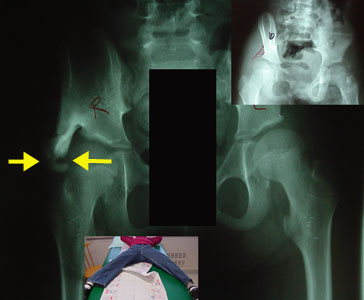 The yellow arrow
points out a "break" in the new bone mass. This demarcates the moving area from the stabilizing area. Nothing actually broke. It is just that the moving region cannot
join the stabilizing area because of the motion performed during healing and bone maturation. The yellow arrow
points out a "break" in the new bone mass. This demarcates the moving area from the stabilizing area. Nothing actually broke. It is just that the moving region cannot
join the stabilizing area because of the motion performed during healing and bone maturation.
Here is another child, one with a Baclofen pump, and severe dystonia whose left hip was
getting gradually more uncovered on each exam.
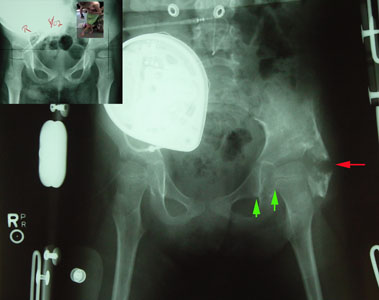 The red arrow shows that the bone below was not allowed to join the bone above by maintaining range of hip motion through the healing bone
formation period. The red arrow shows that the bone below was not allowed to join the bone above by maintaining range of hip motion through the healing bone
formation period.
The green arrows show that although the hip is more centered than before, it is not perfect.
Deepening the hip does not make the hip a normal hip. Long term success will depend on the growth of the hip and whether the hip is kept stable by the extra bone.
 In this case, a substantial early bone awning holds the hip in the shallow socket. We hope that the native socket, so protected, will
deepen as it grows rather than the opposite. The preop image is the smaller inset image which shows the left hip nearly 50% uncovered. In this case, a substantial early bone awning holds the hip in the shallow socket. We hope that the native socket, so protected, will
deepen as it grows rather than the opposite. The preop image is the smaller inset image which shows the left hip nearly 50% uncovered.
 The smaller image shows the S.L.O.B. awning of bone and formation of a deeper native socket seen about 9 months after
the preop image. The smaller image shows the S.L.O.B. awning of bone and formation of a deeper native socket seen about 9 months after
the preop image.
The goal to get the native socket to grow properly seems to be attained - so far. A prospect for growth is required.
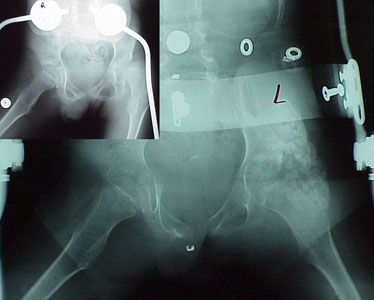 This is a tough one. Despite a popular "abduction" brace, which we see in the preop smaller image, we also see that the hip is not
abducted by the brace. This is very common. Braces that steer wayward legs in walking may fail against sustained spastic or rigid forces. This is a tough one. Despite a popular "abduction" brace, which we see in the preop smaller image, we also see that the hip is not
abducted by the brace. This is very common. Braces that steer wayward legs in walking may fail against sustained spastic or rigid forces.
But the process has gone very far. Remaining growth is limited. Can the appended bone mass, alone,
sustain the hip? We don't know.
We prefer that hips do not get this far gone nor this old before being treated.
A very shallow socket. This is very difficult for any kind of treatment. A "VRO" which points the upper end of the femur into the socket does not have much socket into which to be directed.
If the outcropping awning of bone holds the ball in the limited native socket and then that
socket deepens with growth, then we win. If not, not. But all of the current methods share this problem. We need to sometimes combine procedures or select those that are
more oriented to the worst aspect of the problem. How much femoral anteversion is
present becomes a very important detail in determining which of the choices are to be used.
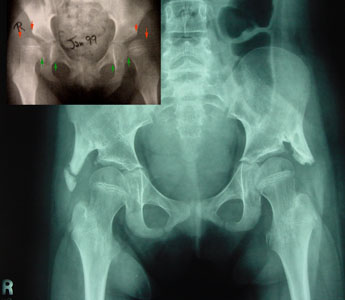 Two immature uncovered (shallow) hips were stabilized by S.L.O.B. surgery early enough for native growth to deepen the native sockets. Two immature uncovered (shallow) hips were stabilized by S.L.O.B. surgery early enough for native growth to deepen the native sockets.
But if femoral anteversion (the rotatory twist of the femur bone) points the ball straight forward, then a severe dislocating twist happens every time the knee points forward.
If femoral anteversion is severe, then derotational surgery of the upper femur (VRO) better targets the dislocation forces.
 The right hip which was heading toward dislocation as the socket became ever shallower deepened. The left untreated
and initially deeper socket has not done as well. The originally more impaired hip socket has become the more stable hip. The right hip which was heading toward dislocation as the socket became ever shallower deepened. The left untreated
and initially deeper socket has not done as well. The originally more impaired hip socket has become the more stable hip.
Should both hips get treatment? We have not practiced preemptive procedures. There is a statistical
possibility of an untreated hip later needing surgery balanced against the potential for complications inherent in any surgery.
 Not quite two years after surgery, the deeper hip shape is evident (horizontal roof). Even so, the tall inner wall of the
older socket tells the history of the prior gradual migration. Not quite two years after surgery, the deeper hip shape is evident (horizontal roof). Even so, the tall inner wall of the
older socket tells the history of the prior gradual migration.
 Both hips quite shallow and uncovered in a young patient are deep and stable with deep native sockets several years after
surgery. On the right side, interestingly, the outcropping bone has absorbed as the native hip appreciably deepened. Both hips quite shallow and uncovered in a young patient are deep and stable with deep native sockets several years after
surgery. On the right side, interestingly, the outcropping bone has absorbed as the native hip appreciably deepened.
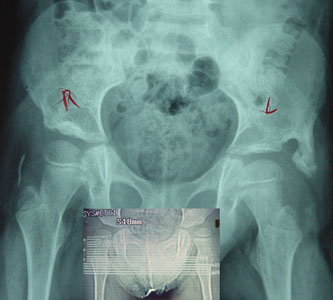
 A left hip way too far gone (small
inset image) with a very shallow and vertical shape. VRO could point the ball more steeply into the socket but that socket is nearly nil. It might work but in severely dystonic
patients it is likely to fail. It was hard to get this much depth with surgery and there is no longer the outcropping we would have desired. But, so far, it is holding and deepening. A left hip way too far gone (small
inset image) with a very shallow and vertical shape. VRO could point the ball more steeply into the socket but that socket is nearly nil. It might work but in severely dystonic
patients it is likely to fail. It was hard to get this much depth with surgery and there is no longer the outcropping we would have desired. But, so far, it is holding and deepening.
An older patient with limited hip growth potential and with dislocation or advanced
subluxation is not a great candidate for the S.L.O.B. (Summit Shelf) procedure. That is just asking too much. We have done the surgery on a few such patients for whom
alternatives were also bad and who desired an attempt at salvage. Results are not encouraging as to the stability gained.
Clearly, the ability to make bone is important. Diseases which deplete bone will deplete
the grafted bone with striking effectiveness. Steroids and multiple anti seizure meds given together can deplete the bone outcropping. We have reversed two such instances by
medical (calcium, Vitamin D) management and by percutaneous injection of the SLOB region (which keeps the collagen even after the calcium departs) with bone morphogenic protein (BMP).
|

